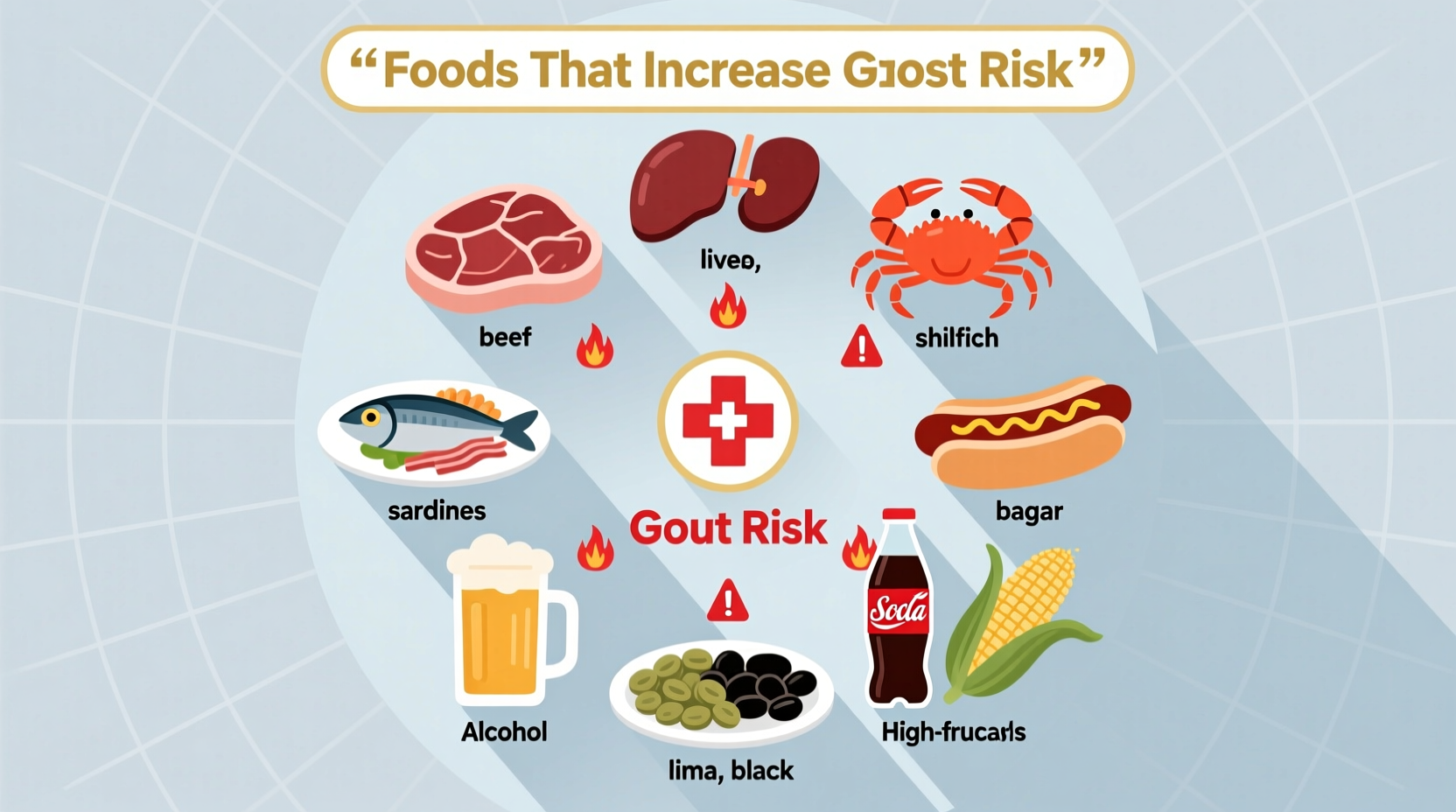
Based on current medical research from the American College of Rheumatology and Mayo Clinic, the top 10 foods that trigger gout are: organ meats, certain seafood (anchovies, sardines), game meats, gravy, beer and liquor, yeast extracts, processed meats, mushrooms, asparagus, and spinach. These high-purine foods increase uric acid levels that cause painful gout flare-ups.
Why Certain Foods Trigger Gout: The Science Simplified
Understanding gout triggers starts with recognizing how your body processes purines. Purines are natural compounds found in many foods that break down into uric acid. When uric acid builds up in your bloodstream, it forms needle-like crystals in your joints, causing the intense pain characteristic of gout attacks.
"Approximately 30% of uric acid in your body comes from dietary sources," explains Dr. Hyon Choi, Director of the Clinical Epidemiology Research Center at Massachusetts General Hospital. "While genetics play a role, dietary choices significantly impact gout flare frequency."

Your Actionable Guide to Gout-Triggering Foods
Immediate Dietary Red Flags
These foods consistently rank highest in purine content according to the National Institutes of Health's dietary database:
| Food Category | Purine Content (mg/100g) | Gout Risk Level |
|---|---|---|
| Organ meats (liver, kidney) | 300-500 | Extreme |
| Anchovies, sardines, mussels | 200-400 | Very High |
| Game meats (venison, rabbit) | 150-300 | High |
| Gravy and meat extracts | 100-250 | High |
| Beer and hard liquor | N/A (alcohol effect) | Very High |
Why Beer Is Particularly Problematic for Gout Sufferers
Research published in The Lancet shows beer increases gout risk more than other alcoholic beverages due to its dual impact: alcohol metabolism competes with uric acid excretion while beer's yeast content provides additional purines. Just two beers daily can triple gout attack risk compared to non-drinkers.
Common Misconceptions About Gout Triggers
Many patients mistakenly avoid all vegetables, but recent research has changed our understanding. A landmark 2020 study in Arthritis & Rheumatology found plant-based purines (from asparagus, spinach, mushrooms) pose significantly lower risk than animal-based purines. The study tracked 5,000 gout patients over five years, revealing:
- Vegetable purines increased gout risk by only 8% compared to 21% for meat purines
- Participants eating moderate vegetable purines had 15% fewer flare-ups than those avoiding them completely
- Fiber content in vegetables may actually help reduce uric acid levels
Practical Dietary Strategies for Gout Management
Instead of complete elimination, focus on these evidence-based approaches:
Smart Substitution Guide
Replace high-risk foods with these gout-friendly alternatives:
- Instead of organ meats: Choose lean chicken or turkey breast (purine content: 50-75mg/100g)
- Instead of beer: Opt for moderate red wine consumption (studies show less impact on uric acid)
- Instead of processed meats: Select fresh fish like salmon 1-2 times weekly (moderate purines with anti-inflammatory benefits)
- Instead of yeast extracts: Use fresh herbs and citrus for flavor enhancement
Timing Matters: When to Be Extra Cautious
Research shows certain situations dramatically increase food trigger risks:
- Dehydration periods: Uric acid concentrates when fluid intake is low - avoid trigger foods when traveling or exercising
- After surgery or illness: Metabolic changes increase gout susceptibility for 2-3 weeks
- During medication changes: Some blood pressure medications interact with purine metabolism
Long-Term Dietary Patterns That Reduce Gout Flare Frequency
A 2022 meta-analysis in The American Journal of Clinical Nutrition identified these dietary patterns associated with 35-50% fewer gout attacks:
- Daily consumption of low-fat dairy products (milk, yogurt)
- Cherries or tart cherry juice (anthocyanins reduce inflammation)
- Complex carbohydrates replacing refined grains
- Hydration with at least 2L of water daily
The Dietary Approaches to Stop Hypertension (DASH) diet, originally designed for blood pressure management, has shown remarkable effectiveness for gout prevention according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
When to Consult Your Healthcare Provider
Dietary changes alone may not control severe gout. Consult your physician if:
- You experience more than two flare-ups annually
- Pain persists beyond 7-10 days despite medication
- You develop tophi (uric acid crystal deposits under skin)
"While diet plays a crucial role, medication remains essential for many patients," advises Dr. John Fitzgerald, rheumatologist at UCLA Medical Center. "The most successful outcomes come from combining appropriate medication with strategic dietary modifications."
Putting It All Together: Your Gout Management Action Plan
Based on current evidence, here's a practical weekly approach:
- Immediate action: Eliminate organ meats and reduce beer consumption
- Weekly planning: Design meals with no more than one high-purine animal protein source per day
- Daily habit: Consume 8-10 glasses of water and include one serving of low-fat dairy
- Monthly check: Monitor flare frequency and discuss patterns with your doctor










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4