Understanding FODMAPs: The Science Behind Digestive Relief
When you're searching for "what are low fodmap foods," you're likely seeking solutions for digestive discomfort. FODMAPs—fermentable oligosaccharides, disaccharides, monosaccharides, and polyols—are short-chain carbohydrates that some people struggle to absorb properly. These poorly absorbed carbs travel to your colon where gut bacteria ferment them, producing gas and drawing in water—leading to the uncomfortable symptoms many with irritable bowel syndrome (IBS) experience.
Developed by researchers at Monash University in Australia, the low FODMAP diet has become the gold standard for managing IBS symptoms. Unlike fad diets, this approach is backed by over a decade of clinical research showing significant symptom improvement in 50-80% of IBS patients. The diet works in three phases: elimination (2-6 weeks), reintroduction (8-12 weeks), and personalization (long-term maintenance).

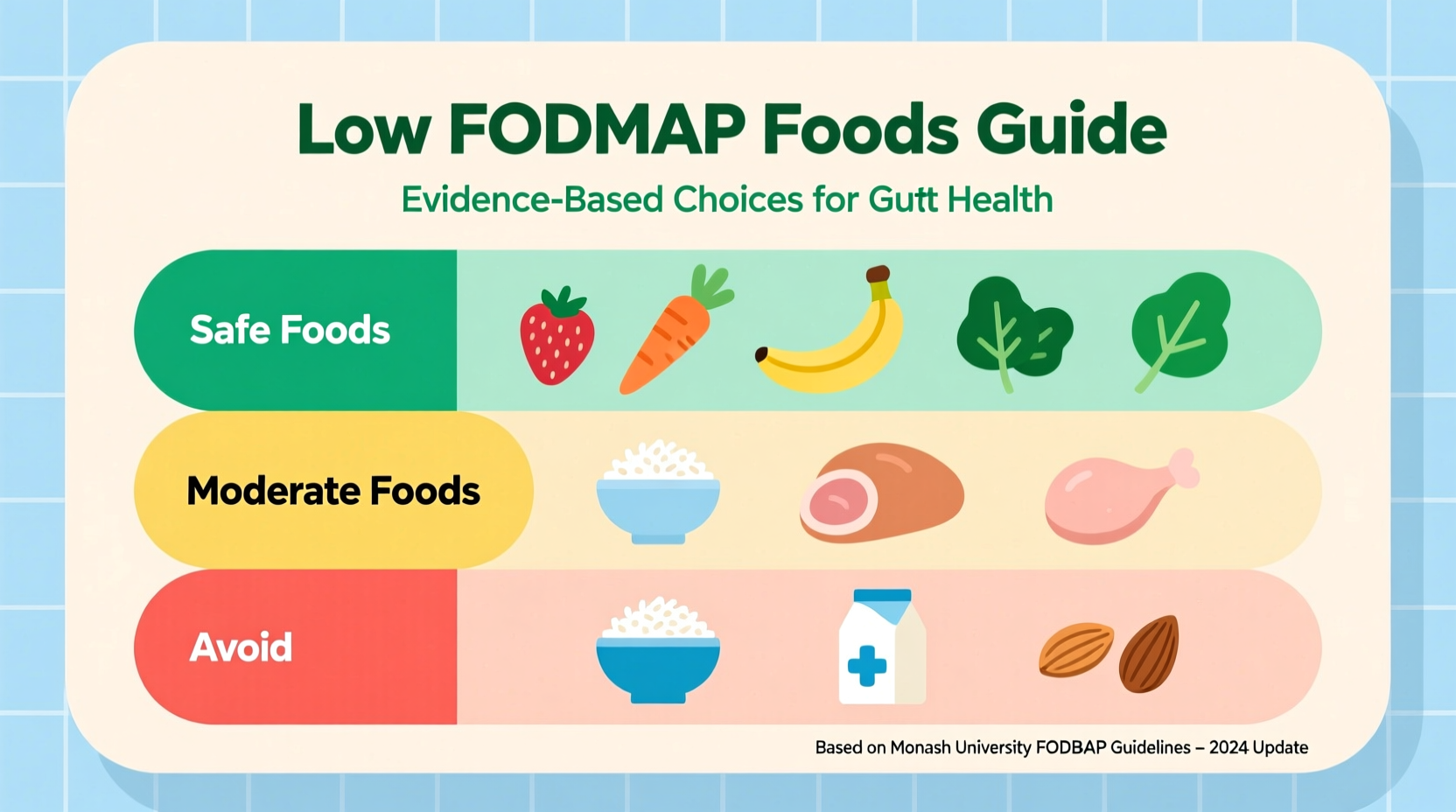
Low FODMAP Food Guide: Your Practical Reference
Navigating which foods qualify as low fodmap foods requires understanding both food categories and appropriate serving sizes. Many nutritious foods contain FODMAPs in amounts that become problematic only when consumed in certain quantities. The following comprehensive reference helps you identify safe options during the elimination phase:
| Food Category | Low FODMAP Options | Safe Serving Size | High FODMAP Foods to Avoid |
|---|---|---|---|
| Fruits | Banana (firm), blueberries, strawberries, oranges | 1 medium fruit or 1 cup | Apples, pears, mango, watermelon |
| Vegetables | Carrots, zucchini, bell peppers, spinach | 1/2 cup cooked or 1 cup raw | Onions, garlic, cauliflower, mushrooms |
| Grains | Oats, quinoa, rice, sourdough spelt bread | 1/2 cup cooked or 1 slice | Wheat bread, barley, rye |
| Proteins | Chicken, fish, eggs, firm tofu | 3-4 oz serving | Beans, lentils, tempeh |
| Dairy | Lactose-free milk, hard cheeses, almond milk | 1 cup or 1 oz | Regular milk, yogurt, soft cheeses |
Implementing Your Low FODMAP Diet Successfully
Starting a low FODMAP diet requires careful planning to ensure nutritional adequacy while eliminating trigger foods. Many people make the mistake of focusing only on what to remove rather than what to include. During the elimination phase, prioritize naturally low FODMAP whole foods rather than relying on specialty products.
When grocery shopping for low fodmap grocery list items, focus on single-ingredient foods and always check labels for hidden high FODMAP ingredients like honey, high fructose corn syrup, and inulin. The Monash University Low FODMAP app provides the most current, research-validated information on food FODMAP content and safe serving sizes.
Meal planning is essential for low fodmap meal prep success. Batch cooking low FODMAP-friendly staples like quinoa, roasted vegetables, and grilled proteins ensures you always have safe options available. For breakfast, try a smoothie with lactose-free milk, spinach, and strawberries. Lunch could feature a quinoa salad with grilled chicken and bell peppers. Dinner might include baked salmon with roasted carrots and zucchini.
Contextual Considerations: When Low FODMAP Works Best
While effective for many, the low FODMAP approach isn't appropriate for everyone. This diet was specifically developed for managing IBS symptoms and shows limited benefit for other digestive conditions. According to the American College of Gastroenterology, the low FODMAP diet is recommended as a second-line therapy after basic dietary modifications have failed to control IBS symptoms.
Important limitations to understand: the elimination phase is intentionally restrictive and should not be maintained long-term. Prolonged restriction can negatively impact gut microbiome diversity. The reintroduction phase is crucial for identifying personal triggers and expanding your dietary variety. Working with a registered dietitian specializing in gastrointestinal nutrition significantly improves outcomes and prevents unnecessary food restrictions.
Research published in Gastroenterology shows that after completing all three phases, most people can tolerate at least some moderate-FODMAP foods, with only 2-3 specific triggers needing long-term avoidance. This personalized approach maintains nutritional balance while effectively managing symptoms.
Long-Term Management and Personalization
The ultimate goal of understanding what are low fodmap foods isn't permanent restriction but rather identifying your personal triggers. After 2-6 weeks of strict elimination, the reintroduction phase systematically tests individual FODMAP groups to determine your specific tolerances. This process typically takes 8-12 weeks and requires careful documentation of symptoms.
During personalization, you'll create your unique low FODMAP diet that includes as many foods as possible while keeping symptoms under control. Most people find they can reintroduce certain FODMAP types at specific thresholds. For example, you might tolerate small amounts of garlic but not onions, or handle lactose but not fructose.
For ongoing success with low fodmap diet tips, consider these strategies:
- Keep a detailed food and symptom journal during reintroduction
- Test one FODMAP group at a time with 3-day intervals
- Start with small test portions and gradually increase
- Work with a dietitian who understands FODMAP thresholds
- Re-test foods periodically as tolerances can change
Remember that digestive health involves more than just diet. Stress management, regular exercise, and adequate sleep all contribute to gut health and can enhance the effectiveness of your low FODMAP approach.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4