When searching for answers about food allergies, getting accurate information matters for your health and safety. This guide delivers evidence-based insights about the most common food allergies, their prevalence patterns, and practical management strategies backed by leading medical authorities. You'll learn not just which allergy tops the charts, but how prevalence shifts across age groups, what symptoms to watch for, and actionable steps to protect yourself or loved ones.
Understanding Food Allergy Prevalence Patterns
Food allergies impact approximately 5.6 million children and 20 million adults in the United States. The Centers for Disease Control and Prevention (CDC) reports a steady increase in food allergy prevalence over the past two decades, with shellfish allergy emerging as the most common among adults. This shift reflects changing dietary patterns, environmental factors, and improved diagnostic capabilities.
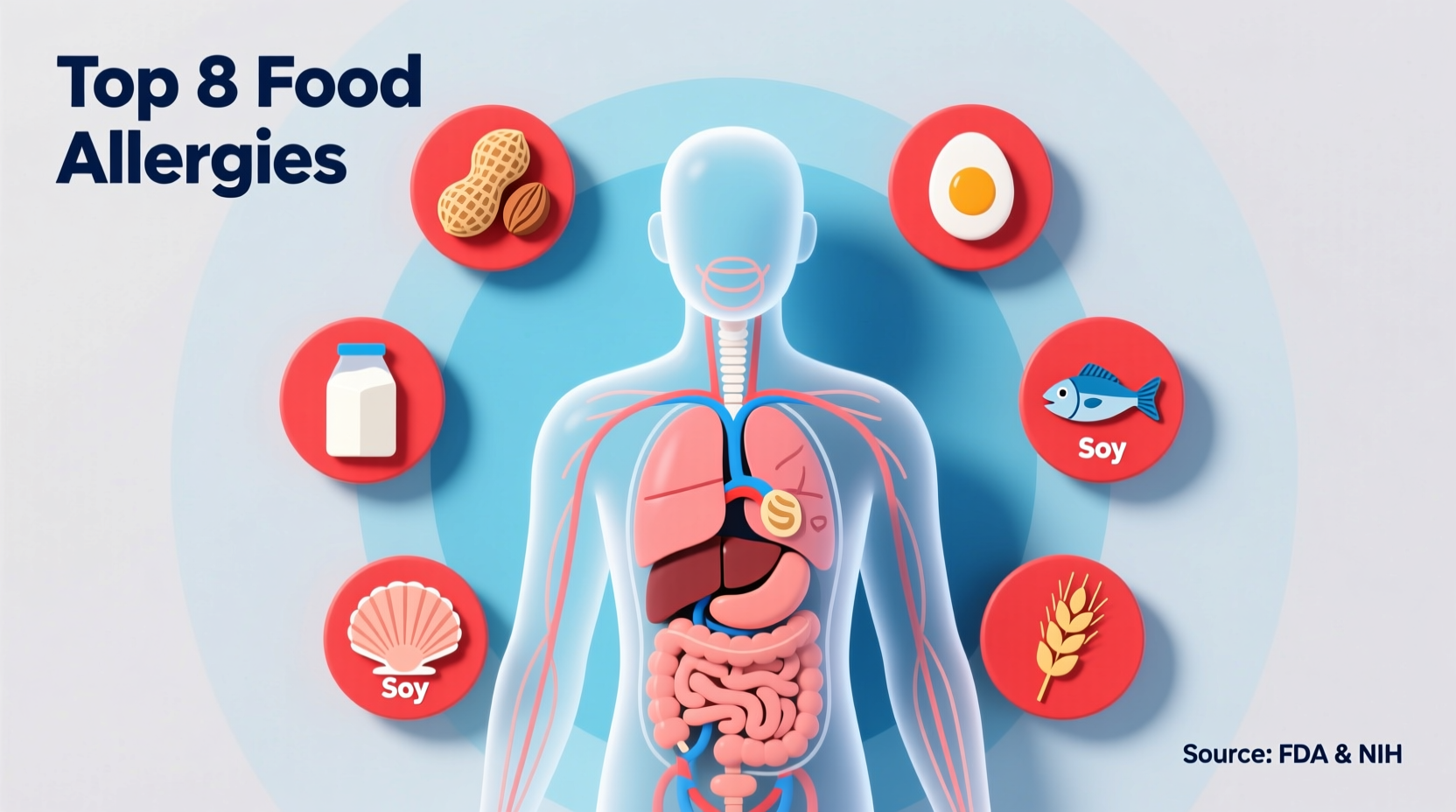
According to the National Institute of Allergy and Infectious Diseases (NIAID), the "Big 9" allergens account for 90% of all food allergy reactions in the United States. These include milk, eggs, fish, crustacean shellfish, tree nuts, peanuts, wheat, soybeans, and sesame. While all pose significant risks, their prevalence varies dramatically across different demographics.
| Allergen | Adult Prevalence | Child Prevalence | Common Sources | Severity Risk |
|---|---|---|---|---|
| Shellfish | 2.3% | 0.5% | Shrimp, crab, lobster | High (anaphylaxis risk) |
| Milk | 1.9% | 2.9% | Dairy products | Medium |
| Peanuts | 1.8% | 2.2% | Peanut butter, baked goods | High |
| Tree Nuts | 1.2% | 1.8% | Almonds, walnuts, cashews | High |
| Eggs | 0.8% | 1.3% | Baked goods, pasta | Medium |
Why Shellfish Tops the Adult Allergy List
Shellfish allergy's dominance among adults stems from several biological and environmental factors. Unlike many childhood allergies that develop early, shellfish allergy frequently appears in adulthood, often after multiple previous exposures. The primary culprit is tropomyosin, a protein found in shellfish that triggers a strong immune response in susceptible individuals.
Research published in the Journal of Allergy and Clinical Immunology reveals that coastal populations show higher shellfish allergy rates than inland communities, suggesting environmental exposure plays a role. Additionally, improved seafood processing and distribution have increased consumption frequency, potentially contributing to rising allergy rates.

Milk Allergy: The Childhood Prevalence Leader
For children under 18, milk allergy claims the top spot in prevalence statistics. The American Academy of Pediatrics explains that immature digestive systems in infants and young children struggle to properly process casein and whey proteins in cow's milk. Approximately 80% of milk-allergic children outgrow their allergy by age 16, unlike shellfish allergy which typically persists throughout life.
Parents should recognize that milk allergy differs from lactose intolerance—a common misconception. While lactose intolerance involves digestive enzyme deficiency, milk allergy triggers an immune system response that can be life-threatening. Symptoms typically appear within minutes to hours after exposure and may include hives, vomiting, or breathing difficulties.
Recognizing and Managing Shellfish Allergy
Shellfish allergy symptoms range from mild to life-threatening. Early warning signs include:
- Itching or tingling in the mouth
- Hives, itching, or eczema
- Swelling of lips, face, tongue, or throat
- Wheezing, nasal congestion, or trouble breathing
- Abdominal pain, diarrhea, nausea, or vomiting
Diagnosis typically involves skin prick tests, blood tests measuring specific IgE antibodies, or supervised oral food challenges conducted by board-certified allergists. The American Academy of Allergy, Asthma & Immunology emphasizes that self-diagnosis can be dangerous and lead to unnecessary dietary restrictions.
Practical Protection Strategies
Living safely with shellfish allergy requires vigilance across multiple environments:
Dining Out Safely
Always inform restaurant staff about your allergy before ordering. Research establishments in advance using allergy-focused apps. Be aware that cross-contamination can occur through shared cooking surfaces, fryers, or utensils. Mediterranean, Asian, and seafood restaurants pose higher risks due to frequent shellfish use in broths and sauces.
Reading Food Labels Effectively
FDA regulations require clear labeling of the "Big 9" allergens. Look for statements like "Contains: Shellfish" or ingredient lists mentioning specific shellfish types. Be cautious with products labeled "may contain shellfish" or "processed in a facility with shellfish," as these indicate potential cross-contamination risks.
Emergency Preparedness
Work with your allergist to develop a personalized emergency action plan. Carry two epinephrine auto-injectors at all times and ensure family members, coworkers, and school staff know how to use them. Wear medical identification jewelry indicating your shellfish allergy.
Regional and Age-Related Variations
Food allergy patterns shift significantly across different demographics. While shellfish dominates in American adults, peanut allergy claims the top spot in countries like the United Kingdom and Canada. Children's allergy profiles evolve dramatically as they age—milk and egg allergies commonly resolve, while shellfish and tree nut allergies typically persist.
A 2022 study in Clinical and Experimental Allergy documented how shellfish allergy prevalence has increased by 44% among American adults since 2004. Researchers attribute this rise to increased seafood consumption, changes in food processing techniques, and potential environmental factors affecting shellfish protein structures.
When to Consult an Allergist
Seek professional evaluation if you experience:
- Recurrent unexplained hives or digestive issues after eating
- Breathing difficulties following food consumption
- Previous mild reactions that may indicate escalating sensitivity
- Family history of severe food allergies
Board-certified allergists can provide accurate diagnosis through comprehensive testing and develop personalized management plans. The National Institute of Allergy and Infectious Diseases recommends early introduction of allergenic foods to infants as a potential prevention strategy for certain food allergies, though this approach requires medical supervision.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4