Understanding food allergies could save your life or someone else's. Each year, food allergies send over 200,000 Americans to emergency rooms, with children under 18 representing nearly half of all cases (CDC, 2023). Whether you're a concerned parent, someone experiencing unexplained symptoms, or simply want to be prepared, recognizing the signs of an allergic reaction is critical knowledge.
How Your Body Reacts: The Science Behind Food Allergies
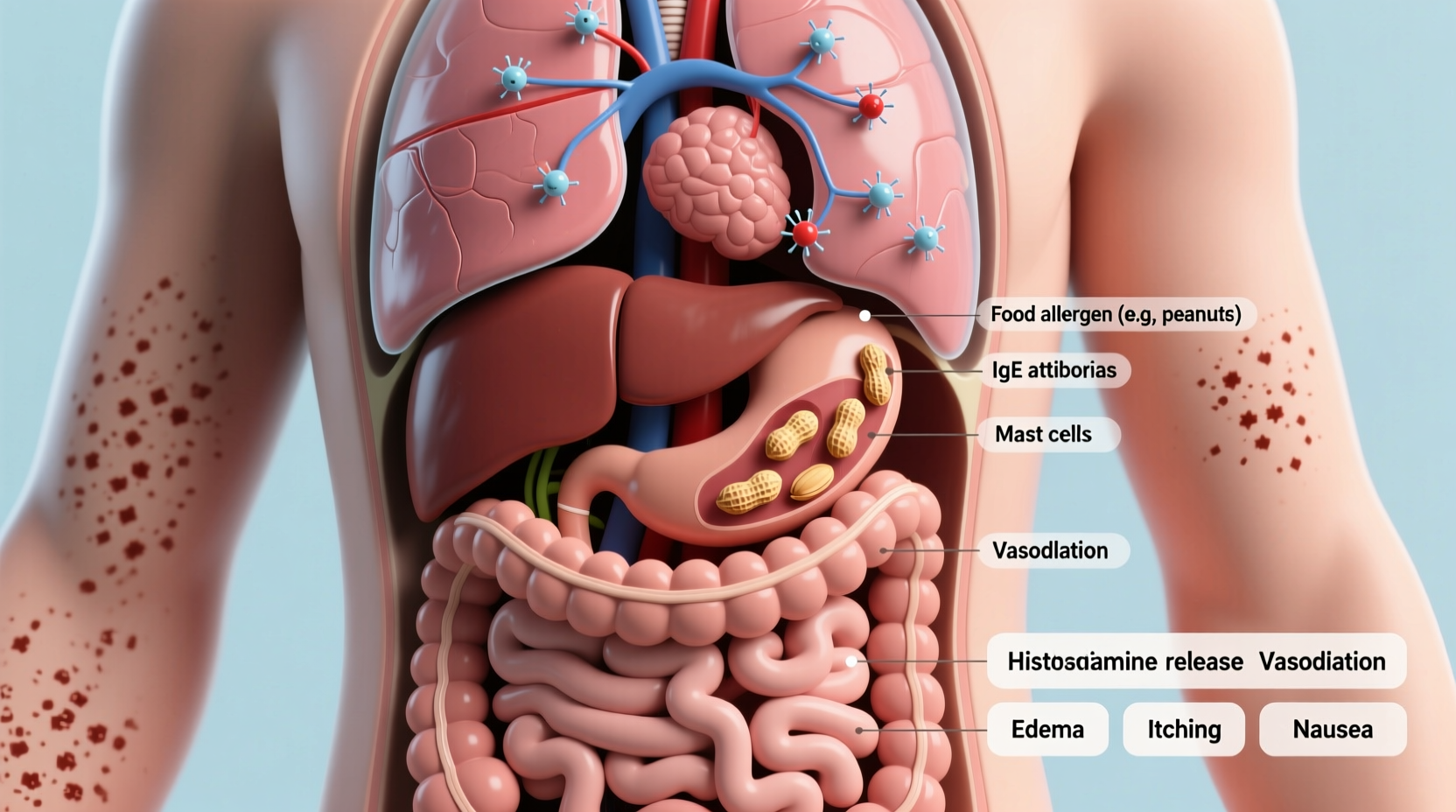
When someone with a food allergy consumes an allergen, their immune system mistakes the protein for a dangerous invader. This triggers immunoglobulin E (IgE) antibodies to release histamine and other chemicals into the bloodstream. Unlike food intolerances—which involve digestive issues—food allergies activate the immune system and can escalate rapidly.
| Food Allergy | Food Intolerance |
|---|---|
| Immune system response | Digestive system issue |
| Triggered by small amounts | Often dose-dependent |
| Can cause anaphylaxis | Never causes anaphylaxis |
| Symptoms appear quickly (minutes) | Symptoms delayed (hours) |
Symptom Recognition: From Mild to Life-Threatening
Food allergy symptoms typically appear within minutes to two hours after exposure. Recognizing the progression is crucial for timely intervention:
- Mild reactions: Itchy mouth, hives, nasal congestion
- Moderate reactions: Abdominal pain, vomiting, facial swelling
- Severe reactions (anaphylaxis): Difficulty breathing, rapid pulse, dizziness, loss of consciousness
The American College of Allergy, Asthma & Immunology reports that 38% of children with food allergies experience severe reactions. Anaphylaxis requires immediate epinephrine administration—every minute counts when airways begin to close.
Common Allergens and At-Risk Populations
While any food can cause an allergic reaction, these eight account for 90% of cases:
- Peanuts (affects 4.2 million Americans)
- Milk (most common in children)
- Eggs
- Tree nuts
- Wheat
- Soy
- Fish
- Shellfish (most common adult-onset allergy)
According to NIH research, peanut allergies have tripled in children since 1997. Meanwhile, shellfish allergies often develop in adulthood, affecting 2.5% of the U.S. population. Asian and Hispanic populations show higher rates of shellfish sensitivity, while peanut allergies are more prevalent among non-Hispanic white children.
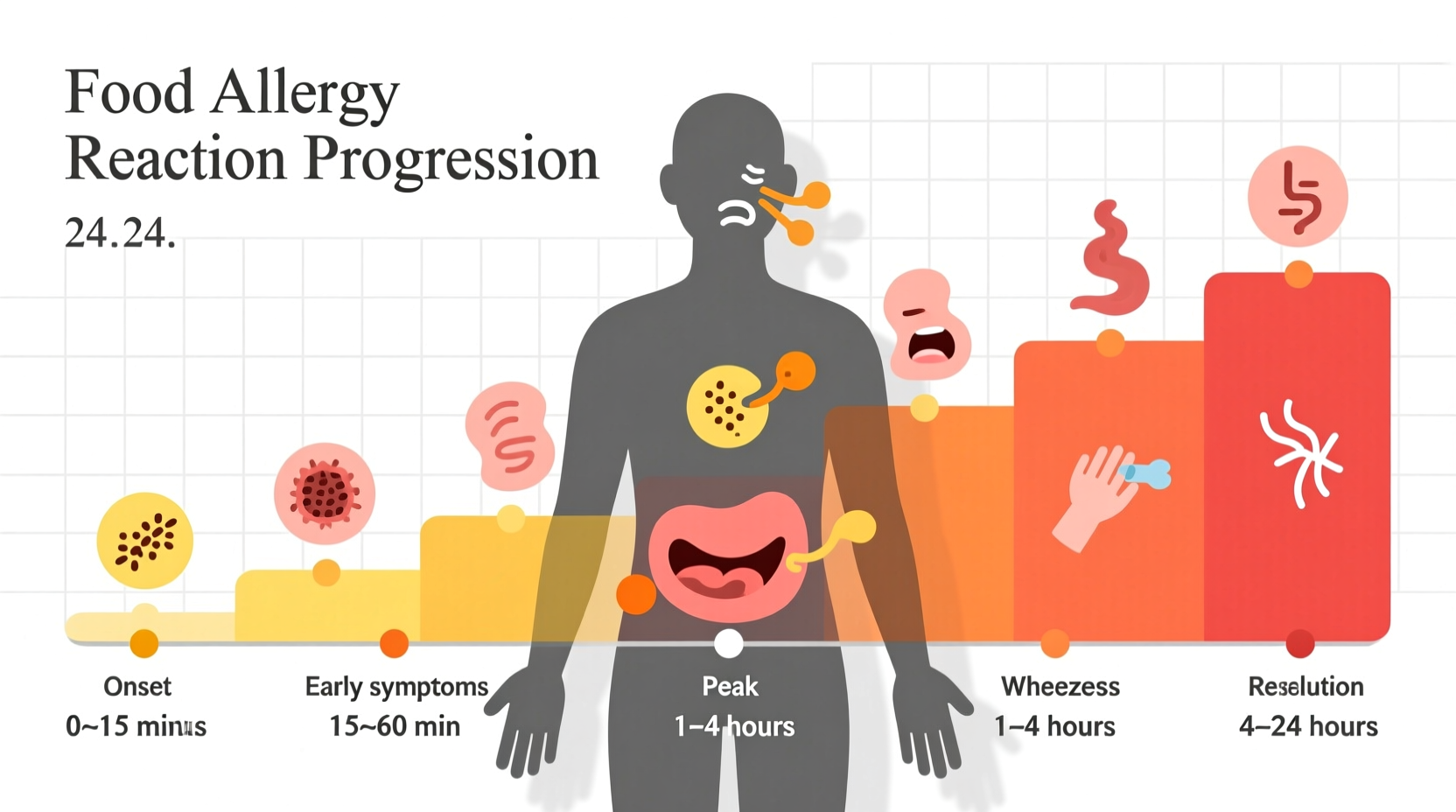
Critical Response Timeline: When Seconds Matter
Understanding the progression of symptoms can mean the difference between recovery and tragedy. The FDA's Food Code outlines this critical timeline:
- 0-30 minutes: Initial symptoms appear (itching, hives)
- 30-60 minutes: Symptoms escalate (swelling, breathing difficulties)
- 60-90 minutes: Anaphylaxis risk peaks (drop in blood pressure, loss of consciousness)
- 90+ minutes: Secondary reaction possible (biphasic response)
Never ignore mild symptoms hoping they'll disappear. The CDC emphasizes that 20% of fatal food allergy reactions occur away from home, often because mild initial symptoms were dismissed. If you carry an epinephrine auto-injector, use it immediately when symptoms suggest an allergic reaction—there's no risk in administering when in doubt.
Diagnosis and Management Strategies
Self-diagnosis of food allergies is dangerous and often inaccurate. Proper diagnosis requires:
- Skin prick tests (90% accurate for common allergens)
- Specific IgE blood tests
- Oral food challenges (gold standard under medical supervision)
Elimination diets should only be conducted with medical guidance to prevent nutritional deficiencies. The National Institute of Allergy and Infectious Diseases confirms that 26% of adults with food allergies develop them to foods they previously consumed without issue—highlighting why ongoing vigilance matters.
Prevention in Daily Life
Managing food allergies requires constant awareness:
- Read all food labels meticulously—even products you've used safely before
- Communicate allergies clearly when dining out (67% of fatal reactions occur in restaurants)
- Carry epinephrine at all times if prescribed
- Educate family, friends, and coworkers about your condition
- Wear medical identification jewelry
The Food Allergy Research & Education organization reports that 40% of children with food allergies experience bullying related to their condition. Creating awareness in schools and workplaces protects not just physical health but emotional well-being too.
When to Seek Emergency Care
Call 911 immediately if you observe:
- Difficulty breathing or wheezing
- Swelling of the throat or tongue
- Sudden drop in blood pressure (pale, weak pulse)
- Loss of consciousness
- Multiple body systems affected (skin + respiratory, for example)
Even if symptoms improve after epinephrine, emergency evaluation is essential—32% of anaphylaxis cases experience a second wave of symptoms hours later. The American Academy of Pediatrics stresses that delayed emergency care increases fatality risk by 50%.
Emerging Treatments and Research
While avoidance remains the primary management strategy, promising developments include:
- Oral immunotherapy (OIT) for peanut allergies (approved for ages 4-17)
- Epinephrine nasal spray (currently in clinical trials)
- Component-resolved diagnostics for more precise testing
- Probiotic research showing potential for prevention
The NIH reports that early introduction of peanut-containing foods to high-risk infants reduces allergy development by 80%. However, always consult an allergist before implementing dietary changes for allergy prevention.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4