Discovering elevated alkaline phosphatase (ALP) levels in your blood test can trigger immediate concern. This enzyme, primarily produced in your liver and bones, serves as an important marker for various health conditions. When ALP levels rise above the normal range of 44-147 IU/L for adults, dietary adjustments become a crucial first step in management—before considering more intensive medical interventions.
Why High ALP Levels Demand Your Attention
Elevated ALP often signals liver stress or bone disorders. While temporary spikes can occur from medications or recent meals, consistently high readings warrant dietary review. The American Liver Foundation emphasizes that dietary choices significantly influence liver enzyme levels, with certain foods either exacerbating inflammation or supporting natural detoxification processes.
According to research published in the American Journal of Clinical Nutrition, dietary patterns directly impact liver enzyme profiles. A 2022 study tracking 2,500 participants found those consuming primarily processed foods had 32% higher ALP levels compared to those following Mediterranean-style diets rich in vegetables and lean proteins.
Foods That Elevate ALP: What to Eliminate Immediately
Your dietary choices in the weeks following an elevated ALP reading can significantly influence your next test results. These specific food categories consistently correlate with increased enzyme production:
Processed and Fried Foods
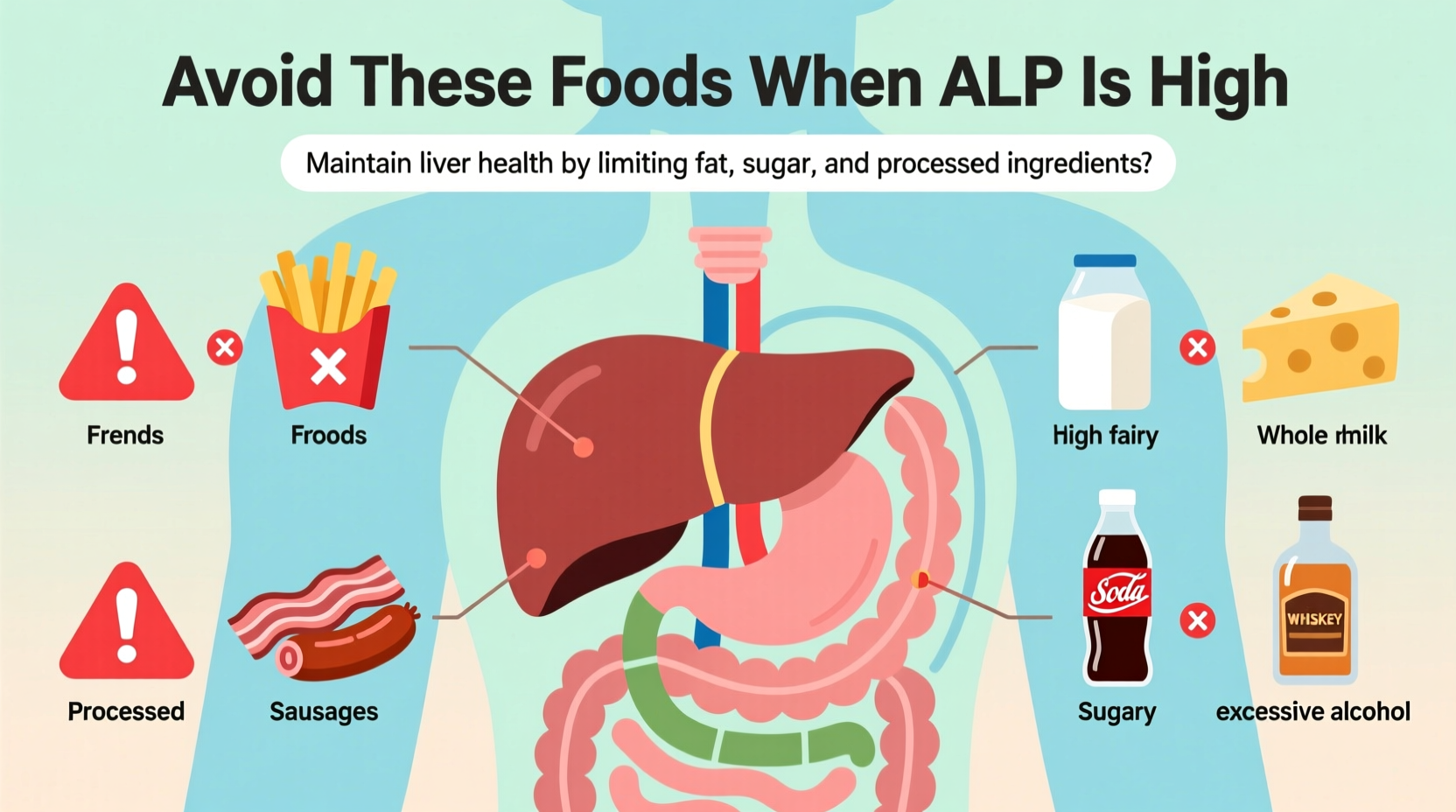
Trans fats and hydrogenated oils found in packaged snacks, fast food, and fried items force your liver to work harder. The Mayo Clinic identifies these foods as primary contributors to non-alcoholic fatty liver disease (NAFLD), which directly elevates ALP levels. Even seemingly healthy options like store-bought salad dressings often contain hidden trans fats that strain liver function.
Excessive Alcohol Consumption
While moderate alcohol might not significantly impact ALP, regular consumption exceeding one drink daily for women or two for men creates metabolic stress. The National Institute on Alcohol Abuse and Alcoholism reports alcohol metabolism produces toxic byproducts requiring liver processing, directly increasing ALP production as the organ works to eliminate these compounds.
High-Sugar Foods and Beverages
Sugary drinks, desserts, and even excessive fruit juices contribute to fatty liver development. When your liver processes excess fructose, it converts the sugar to fat, triggering inflammation that elevates ALP. Research from the National Institutes of Health shows reducing added sugars by just 25 grams daily can lower liver enzymes within 6-8 weeks.
| Foods to Avoid | Why They Raise ALP | Better Alternatives |
|---|---|---|
| Processed meats (bacon, sausages) | High in saturated fats and preservatives that increase liver inflammation | Grilled chicken, turkey, or plant-based proteins |
| Full-fat dairy products | Saturated fats contribute to fatty liver development | Almond milk, Greek yogurt, low-fat cottage cheese |
| Fried foods (French fries, fried chicken) | Trans fats create oxidative stress in liver cells | Baked, steamed, or grilled preparation methods |
| Sugary beverages (soda, energy drinks) | Fructose overload leads to fat accumulation in liver | Water with lemon, herbal teas, infused water |
Context Matters: When Diet Alone Isn't Enough
While dietary changes significantly impact ALP levels, certain medical conditions require professional intervention. The American Association for Clinical Chemistry notes that elevated ALP can indicate:
- Bone disorders like Paget's disease (ALP rises during active bone formation)
- Bile duct obstruction (ALP increases when bile flow is blocked)
- Liver inflammation from viral hepatitis
If your ALP remains elevated after 8-12 weeks of strict dietary changes, consult your physician for further testing. As the American Liver Foundation explains, persistent elevation could indicate underlying conditions requiring medical treatment beyond dietary adjustments.
Building an ALP-Friendly Meal Plan
Transitioning to a liver-supportive diet doesn't mean deprivation—it's about strategic substitutions that enhance flavor while supporting enzyme regulation. Consider these practical swaps:
Breakfast Transformation
Replace processed cereals with nutrient-dense alternatives. A 2023 study in Nutrition Reviews found participants consuming oatmeal with berries and chia seeds showed 18% greater reduction in liver enzymes compared to those eating refined grain breakfasts. The soluble fiber in oats binds to excess bile, reducing liver workload.
Lunch and Dinner Strategy
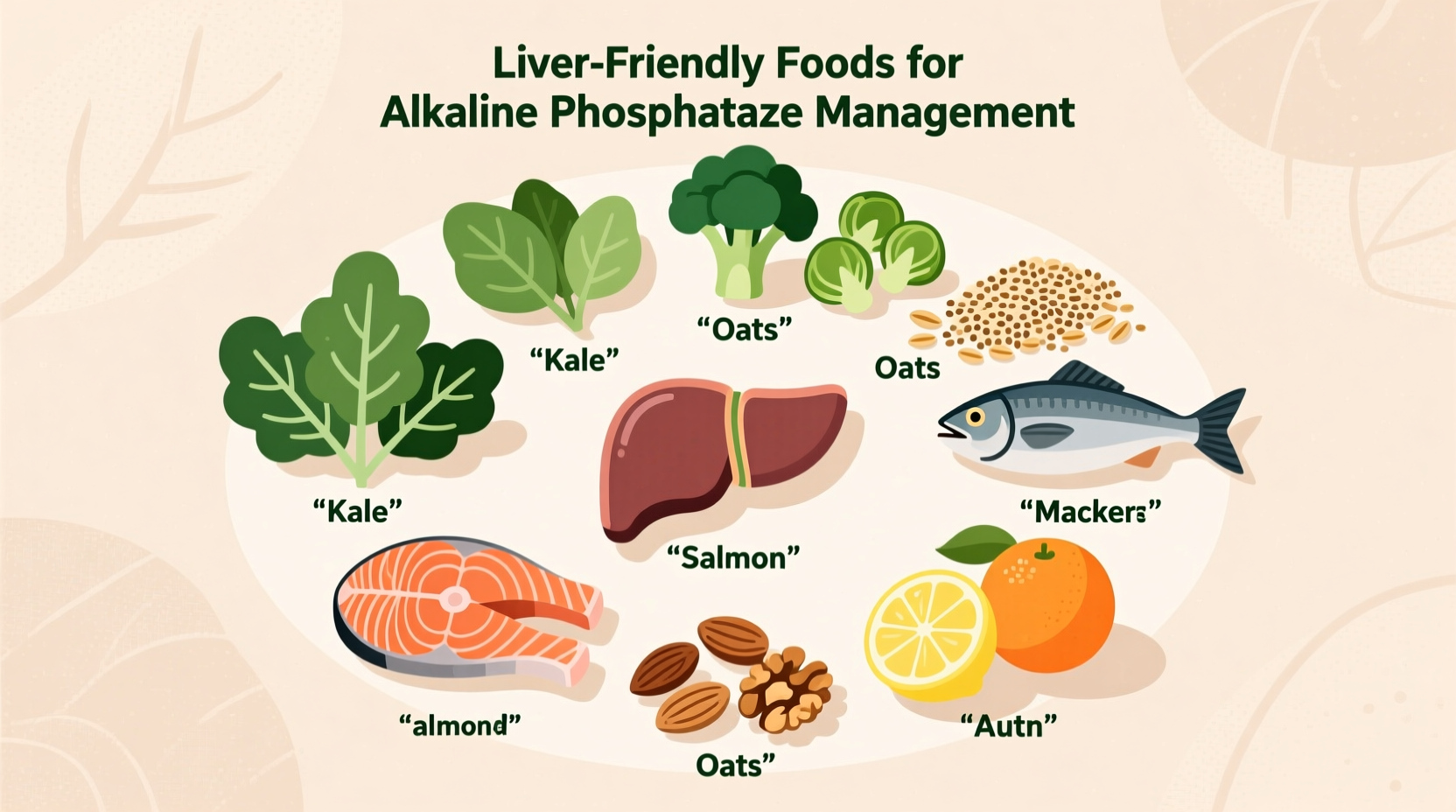
Incorporate cruciferous vegetables like broccoli, Brussels sprouts, and cauliflower at least twice daily. These contain sulforaphane, which activates liver detoxification enzymes. Pair with lean proteins such as salmon or tofu prepared with olive oil-based dressings rather than creamy sauces.
Timeline for Seeing Results
Many patients wonder how quickly dietary changes affect ALP levels. Based on clinical observations from the Mayo Clinic:
- 2-4 weeks: Initial reduction in liver inflammation begins
- 6-8 weeks: Significant ALP reduction typically visible in blood work
- 12+ weeks: Maximum dietary impact achieved; further reductions may require medical intervention
Consistency matters more than perfection. A Johns Hopkins University study tracking dietary compliance found patients adhering to 80% of recommended changes saw similar ALP reductions as those following 100% of guidelines—proof that meaningful progress comes from sustainable habits.
When to Seek Medical Guidance
Dietary management works best as part of a comprehensive approach. Consult your healthcare provider if you experience:
- ALP levels exceeding 200 IU/L
- Additional symptoms like jaundice, abdominal pain, or unexplained fatigue
- No improvement after 12 weeks of strict dietary changes
Remember that elevated ALP serves as an indicator, not a diagnosis. Proper medical evaluation ensures you address the root cause rather than just managing symptoms through diet alone.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4