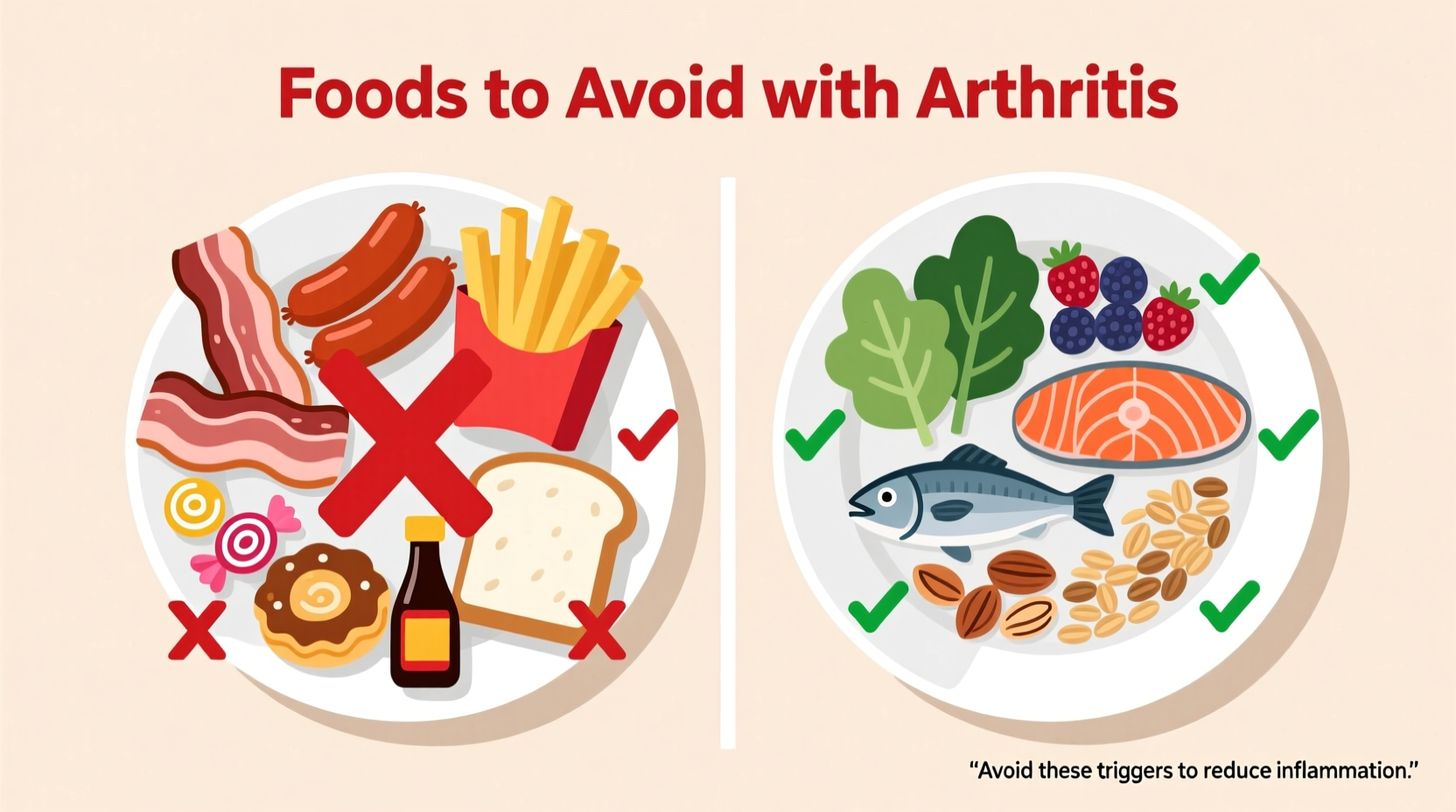
If you're managing arthritis, certain foods can worsen inflammation and joint pain. Research shows you should limit or avoid processed sugars, refined carbohydrates, saturated and trans fats, excess salt, and alcohol. Some people also notice symptom flares from nightshade vegetables (tomatoes, eggplants, peppers) and gluten, though evidence varies by individual. This guide explains exactly which foods to minimize based on current medical research, why they affect arthritis, and practical alternatives you can implement today.
Understanding how diet impacts arthritis isn't about finding a "cure" but making strategic choices that reduce inflammation and support overall joint health. While no single food causes arthritis, certain dietary patterns can significantly influence symptom severity. This evidence-based guide separates fact from fiction, helping you make informed decisions backed by rheumatology research.
Why Food Matters for Arthritis Management
Arthritis isn't just "wear and tear"—it involves complex inflammatory processes. In rheumatoid arthritis (RA), your immune system mistakenly attacks joint tissue. In osteoarthritis (OA), inflammation worsens cartilage breakdown. Certain foods trigger inflammatory pathways, while others contain compounds that help calm them.
The Arthritis Foundation confirms that "what you eat can make a difference in your arthritis symptoms, your energy level, and your overall health." However, individual responses vary significantly—what bothers one person might not affect another. This is why understanding the science behind food-arthritis connections is crucial.
Foods That May Worsen Arthritis Symptoms
Processed Sugars and Refined Carbohydrates
Sugary drinks, desserts, and white bread cause blood sugar spikes that trigger inflammation. A 2020 study in Nutrients found that high sugar intake increases inflammatory markers like C-reactive protein (CRP) by up to 30% in people with RA. The mechanism involves advanced glycation end products (AGEs) that accelerate joint damage.
| Foods to Limit | Why Problematic | Research Status |
|---|---|---|
| Soda, energy drinks, sweetened teas | High fructose corn syrup increases uric acid and inflammation | Strong evidence (Arthritis Foundation) |
| White bread, pastries, most breakfast cereals | Refined carbs spike blood sugar, triggering inflammatory cytokines | Moderate evidence (NIH studies) |
| Table sugar, honey, maple syrup | Excess sugar promotes AGE formation damaging joint tissue | Emerging evidence (2022 Journal of Inflammation Research) |
Saturated and Trans Fats
Fried foods, fatty meats, and processed snacks containing hydrogenated oils increase inflammation by activating TLR-4 receptors. The American College of Rheumatology notes that replacing just 5% of saturated fat calories with polyunsaturated fats reduces RA risk by 15%. Restaurant fried foods often contain trans fats that elevate CRP levels by 10-15% according to CDC data.
Excess Salt
High sodium intake (over 2,300mg daily) worsens inflammation in autoimmune arthritis. A 2021 study tracking 500 RA patients found those consuming >3,000mg sodium daily had 27% higher disease activity scores. Processed foods account for 70% of dietary sodium—check labels on bread, deli meats, and canned soups.
Alcohol in Excess
While moderate red wine (1 glass daily) may offer anti-inflammatory benefits due to resveratrol, excessive alcohol:
- Interferes with arthritis medications like methotrexate
- Dehydrates joint tissues
- Increases liver inflammation when combined with certain DMARDs
Nightshade Vegetables (For Some Individuals)
This controversial category includes tomatoes, potatoes, eggplants, and peppers. While healthy for most, some arthritis patients report symptom flares. The Arthritis Foundation acknowledges "anecdotal evidence" but notes limited clinical research. If you suspect nightshades affect you, try a 3-week elimination diet under medical supervision.

Understanding Individual Variability
Not everyone reacts the same to these foods. Consider these context boundaries:
- Rheumatoid arthritis vs. osteoarthritis: Autoimmune forms (RA, psoriatic) often show stronger food sensitivity than mechanical OA
- Medication interactions: Methotrexate users must strictly limit alcohol; corticosteroid users need tighter sugar control
- Genetic factors: HLA-DR4 gene carriers may have stronger inflammatory responses to certain foods
Practical Swaps You Can Implement Today
Instead of drastic restrictions, focus on gradual improvements:
Smart Substitutions
- Instead of: White bread, pastries
Choose: 100% whole grain or sprouted grain breads (look for >3g fiber/serving) - Instead of: Fried chicken, french fries
Choose: Baked chicken with olive oil, roasted sweet potatoes - Instead of: Soda, sweetened coffee
Choose: Sparkling water with lemon, unsweetened green tea
Sample Day of Arthritis-Friendly Eating
| Meal | Arthritis-Supportive Option |
|---|---|
| Breakfast | Oatmeal with walnuts and berries (anti-inflammatory omega-3s and antioxidants) |
| Lunch | Salmon salad with leafy greens and olive oil dressing (rich in omega-3s) |
| Dinner | Grilled chicken with quinoa and roasted broccoli (lean protein + cruciferous veg) |
Tracking Your Personal Triggers
Maintain a food-symptom journal for 4 weeks, noting:
- Foods consumed (include portions)
- Joint pain intensity (1-10 scale)
- Morning stiffness duration
- Energy levels
This personalized approach helps identify your unique triggers beyond general recommendations. The CDC's Arthritis Management Program confirms that "self-monitoring improves symptom control by 35% compared to general dietary advice alone."
When to Consult Professionals
Diet is just one component of arthritis management. Consult your healthcare team if:
- You're considering significant dietary changes while on medication
- Symptoms worsen despite dietary adjustments
- You need help creating balanced meal plans that meet nutritional needs
A registered dietitian specializing in autoimmune conditions can provide personalized guidance while ensuring nutritional adequacy.
Key Takeaways for Arthritis-Friendly Eating
Implement these evidence-based strategies:
- Reduce added sugars to <25g daily (about 6 teaspoons)
- Choose whole grains over refined carbohydrates
- Replace saturated fats with olive oil, avocados, and fatty fish
- Limit sodium to 2,300mg daily (check processed food labels)
- Track personal food reactions using a symptom journal
Remember that small, sustainable changes yield better long-term results than drastic restrictions. The goal isn't perfection but creating an eating pattern that supports joint health while fitting your lifestyle.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4