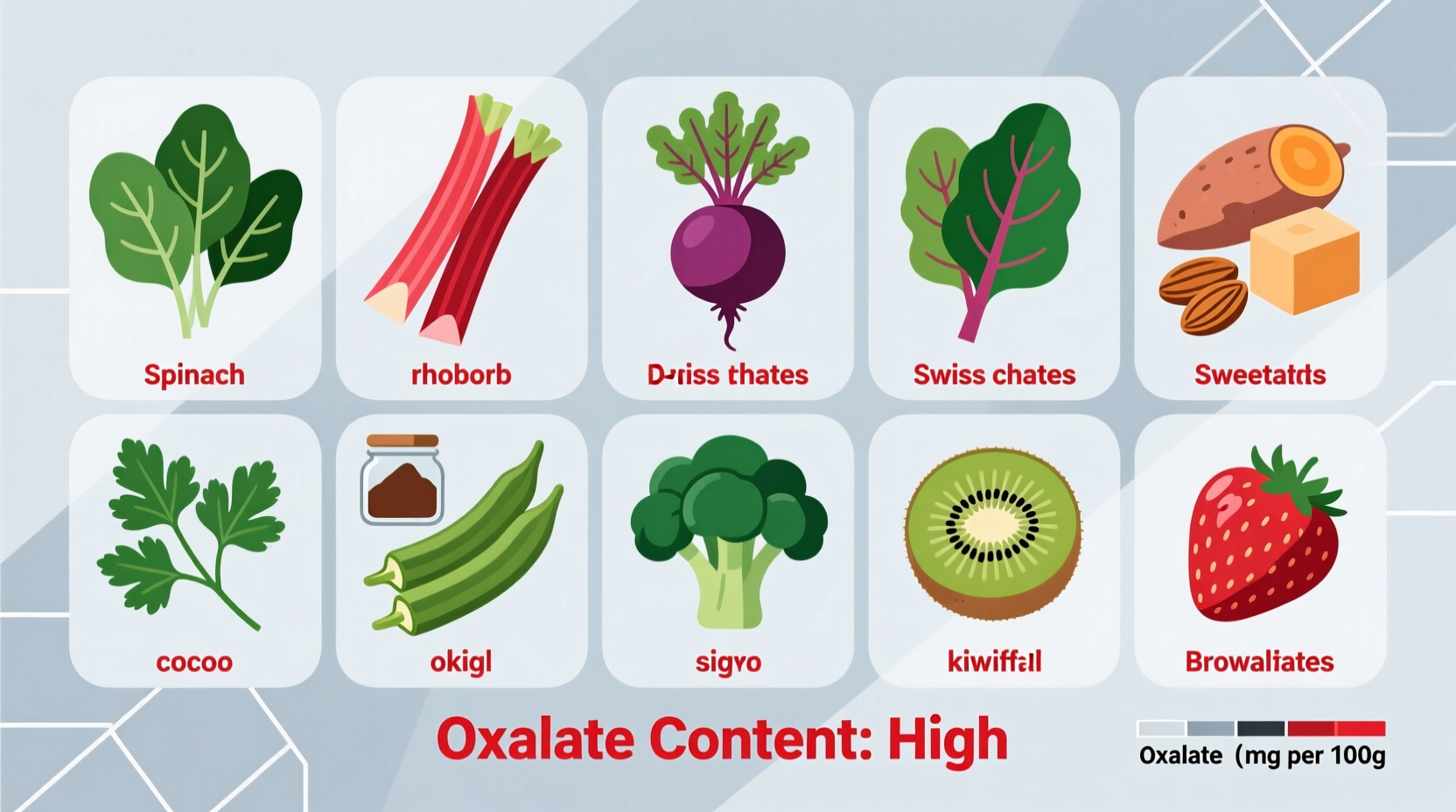
If you're concerned about oxalate intake, the top high-oxalate foods include spinach, rhubarb, beets, Swiss chard, almonds, and soy products. For kidney stone prevention, limiting foods with over 10mg of oxalate per serving is often recommended by healthcare providers. This comprehensive guide details exactly which foods contain high levels of oxalates, provides practical dietary guidance, and explains who should be concerned about oxalate consumption based on current medical understanding.
Understanding which foods are high in oxalates is crucial for anyone managing kidney stones, certain digestive conditions, or following a specialized therapeutic diet. Oxalates are naturally occurring compounds found in many plant-based foods that can contribute to kidney stone formation in susceptible individuals. While most people process oxalates without issues, approximately 1 in 10 Americans will develop kidney stones in their lifetime, making this dietary knowledge essential preventative healthcare.
Why Oxalate Content Matters for Your Health
Oxalates (or oxalic acid) are organic compounds plants produce as part of their natural defense system. When consumed, they can bind with calcium in your digestive tract and form crystals that may develop into kidney stones in predisposed individuals. According to the National Institute of Diabetes and Digestive and Kidney Diseases, calcium oxalate stones represent about 80% of all kidney stones.
"The relationship between dietary oxalate and kidney stone formation is complex," explains Dr. John Asplin, a nephrologist and kidney stone specialist. "While only 10-15% of urinary oxalate comes from diet for most people, those with certain metabolic conditions or a history of calcium oxalate stones may need to monitor high-oxalate foods more carefully."

High-Oxalate Foods: The Complete Reference List
When evaluating oxalate content, researchers typically categorize foods as high (greater than 10mg per serving), moderate (5-10mg), or low (less than 5mg). The following comprehensive list focuses on foods containing significant oxalate levels that may require moderation for at-risk individuals.
| Food Category | Specific Foods | Approximate Oxalate Content (per serving) |
|---|---|---|
| Leafy Greens | Spinach, Swiss chard, beet greens, rhubarb | Spinach: 600-800mg/cup cooked; Rhubarb: 500mg/cup |
| Nuts & Seeds | Almonds, cashews, peanuts, sesame seeds, tahini | Almonds: 122mg/ounce; Tahini: 145mg/2Tbsp |
| Legumes | Soy products, baked beans, refried beans | Soybeans: 200mg/cup; Tofu: varies by preparation |
| Grains | Bran cereals, wheat germ | Bran flakes: 80mg/1/2 cup |
| Fruits | Star fruit, blackberries, raspberries, kiwi | Star fruit: extremely high; Blackberries: 10-15mg/cup |
| Vegetables | Beets, okra, sweet potatoes, potatoes with skin | Beets: 60-150mg/cup; Okra: 80mg/cup |
| Beverages | Tea (especially black), cocoa, chocolate milk | Black tea: 20-100mg/cup; Hot chocolate: 20-50mg/cup |
Context Matters: Who Should Monitor Oxalate Intake
Not everyone needs to restrict oxalate-rich foods. Understanding your personal risk factors helps determine if this dietary information applies to you:
- History of calcium oxalate kidney stones: For recurrent stone formers, dietary modification often becomes part of prevention protocols
- Primary hyperoxaluria: A rare genetic disorder requiring strict oxalate management
- Malabsorption conditions: Including gastric bypass surgery, Crohn's disease, or chronic pancreatitis
- Calcium deficiency: Low calcium intake can increase oxalate absorption
According to research published in the Clinical Journal of the American Society of Nephrology, only about 40% of urinary oxalate comes directly from dietary sources for most people. The liver produces the majority of oxalate in our bodies, which explains why dietary restriction alone doesn't prevent stones for everyone.
Practical Dietary Strategies for Managing Oxalate Intake
If you need to moderate your oxalate consumption, these evidence-based strategies can help without unnecessarily restricting your diet:
Smart Food Preparation Techniques
How you prepare high-oxalate foods significantly impacts their oxalate content:
- Boiling vegetables: Reduces soluble oxalates by 30-90% as oxalates leach into cooking water (which should be discarded)
- Avoiding raw high-oxalate greens: Cooking spinach reduces oxalate bioavailability compared to consuming it raw
- Pairing with calcium-rich foods: Consuming calcium sources (dairy, fortified plant milks) with meals binds oxalates in the gut
Balanced Approach to Dietary Management
Rather than eliminating entire food groups, nutrition experts recommend:
- Moderation over elimination: Most therapeutic diets allow 50-100mg of oxalate daily rather than complete avoidance
- Strategic food combining: Having calcium-containing foods with high-oxalate meals reduces absorption
- Hydration focus: Drinking sufficient water (at least 2.5L daily) dilutes urine concentration
- Gradual changes: Work with a registered dietitian to implement sustainable dietary modifications
The Academy of Nutrition and Dietetics emphasizes that overly restrictive diets can lead to nutrient deficiencies. Their position paper notes that "a balanced approach focusing on overall dietary patterns rather than single nutrients typically yields better long-term outcomes for kidney stone prevention."
Evolving Understanding of Dietary Oxalates
Research on oxalates has evolved significantly over the past two decades. In the early 2000s, blanket recommendations to avoid all high-oxalate foods were common. However, more recent studies reveal a more nuanced picture:
- 2002: Early research suggested strict oxalate restriction for all kidney stone formers
- 2010: Studies showed only 40-50% of urinary oxalate comes from diet for most people
- 2015: Research highlighted the importance of calcium intake alongside oxalate management
- 2020: Current guidelines emphasize personalized approaches based on individual metabolism
This evolution demonstrates why working with healthcare providers who stay current with research is essential for proper dietary management.
When to Consult a Healthcare Professional
While this guide provides general information, personalized medical advice is crucial if:
- You've experienced kidney stones or have been diagnosed with hyperoxaluria
- You're considering significant dietary changes for medical reasons
- You have digestive conditions affecting nutrient absorption
- You're unsure whether oxalate restriction applies to your situation
Registered dietitians specializing in renal nutrition can provide tailored meal plans that maintain nutritional balance while addressing oxalate concerns. The National Kidney Foundation recommends working with professionals who understand both the science of oxalate metabolism and practical dietary implementation.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4