If you're managing gout, your dietary choices directly impact how often you experience those excruciating joint attacks. As someone who has helped countless clients navigate gout-friendly eating through practical food chemistry knowledge, I've seen how strategic dietary changes can transform quality of life. This guide delivers actionable, evidence-based food recommendations that actually work in real-world kitchens—not just theoretical advice from a lab.
Why Certain Foods Trigger Gout Attacks
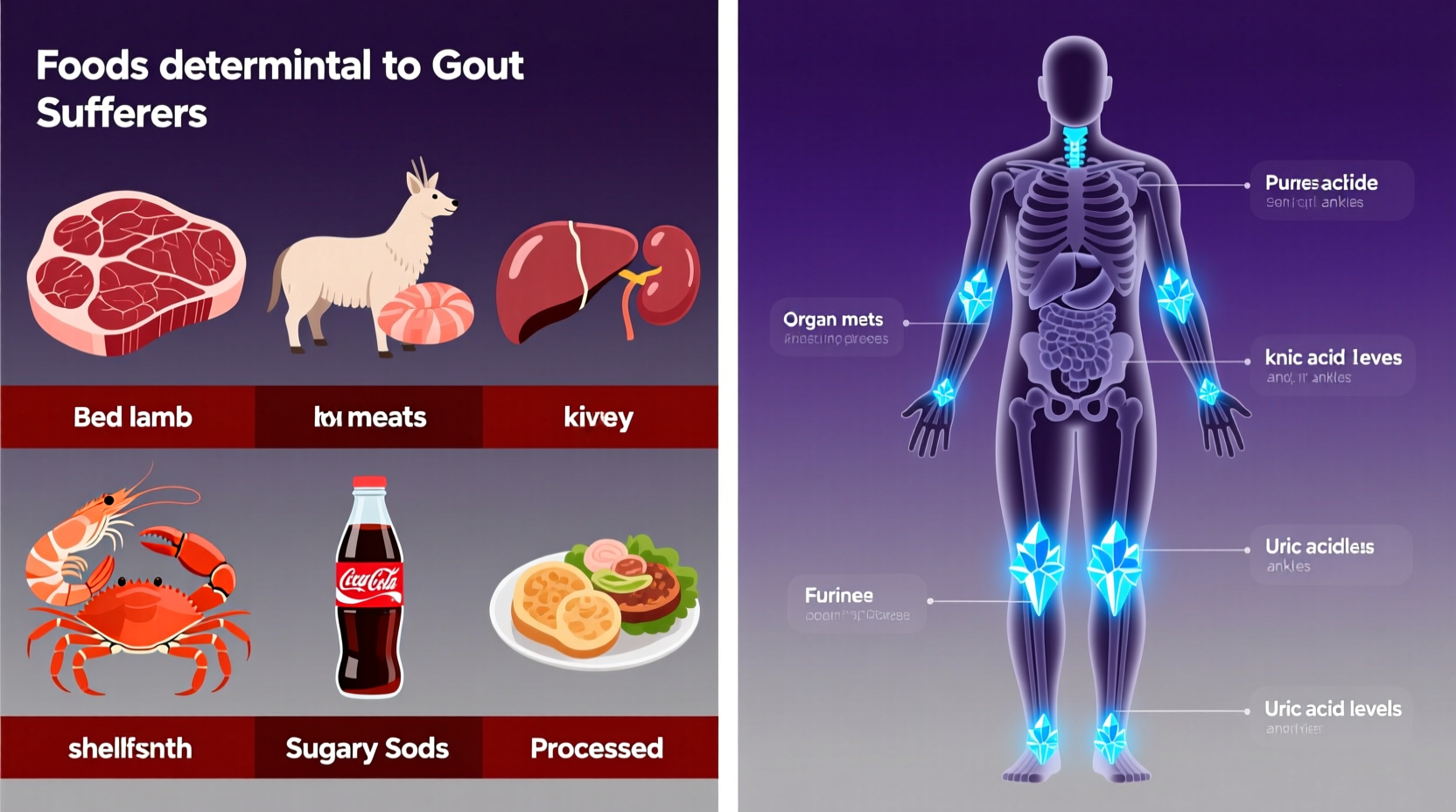
Gout occurs when uric acid crystals accumulate in your joints, causing intense pain and inflammation. Uric acid forms when your body breaks down purines—natural compounds found in certain foods. When uric acid levels exceed 6.8 mg/dL, crystals can form. Research from the American College of Rheumatology shows that dietary choices influence approximately 12% of uric acid levels, making food selection a critical management tool.
Immediate Dietary Triggers: Foods That Cause Rapid Uric Acid Spikes
These foods contain exceptionally high purine concentrations that can trigger flare-ups within 24-48 hours of consumption:
| Food Category | Purine Content (mg/100g) | Uric Acid Impact |
|---|---|---|
| Organ Meats (Liver, Kidney) | 300-400 | ↑↑↑ Extreme risk - avoid completely |
| Anchovies & Sardines | 250-350 | ↑↑↑ High risk - limit to 1oz weekly |
| Beer (all types) | N/A | ↑↑↑ Alcohol + yeast = double impact |
| High-Fructose Corn Syrup | N/A | ↑↑ Rapidly increases uric acid production |
Everyday Foods With Hidden Risks
You don't need to eliminate all animal proteins, but portion control and frequency matter significantly. According to Mayo Clinic research, these common foods require careful management:
- Red meat consumption - Limit to 4-6 ounces maximum, 2-3 times weekly. Beef and lamb contain moderate purines (150-200mg/100g) that accumulate with frequent consumption
- Alcoholic beverages - Beer poses the greatest risk due to yeast content, but all alcohol reduces uric acid excretion. The National Institutes of Health recommends complete avoidance during active flare-ups
- Sugary beverages - Just one 12oz soda daily increases gout risk by 50% according to a 20-year Harvard study tracking 47,000 men

Surprising Dietary Pitfalls
Many gout sufferers unknowingly consume problematic foods through these common channels:
- Yeast extracts - Found in Marmite, Vegemite, and some broths, these contain concentrated purines from yeast fermentation
- Processed foods - Many contain hidden high-fructose corn syrup in unexpected places like bread, sauces, and salad dressings
- Protein supplements - Some whey protein powders contain added yeast or high-purine ingredients that counteract their health benefits
Practical Implementation Strategies
Transitioning to a gout-friendly diet doesn't mean deprivation—it means smarter choices. Implement these kitchen-tested techniques:
- Read labels systematically - Scan for high-fructose corn syrup, yeast extract, and autolyzed yeast in ingredient lists
- Adopt the 80/20 protein rule - 80% of your protein from low-purine sources (eggs, dairy, most vegetables), 20% from moderate-purine options
- Modify cooking methods - Boiling meats reduces purine content by 30-50% compared to grilling or frying
- Create emergency meal templates - Have 3-4 go-to low-purine meals ready for when you feel a flare-up coming
When to Consult Healthcare Professionals
Dietary changes work best alongside medical treatment. Consult your doctor if:
- You experience more than two flare-ups monthly despite dietary changes
- Your uric acid levels remain above 6.0 mg/dL after 3 months of dietary management
- You develop tophi (uric acid crystal deposits under the skin)
Remember that individual responses vary—what triggers one person might not affect another. The Arthritis Foundation recommends keeping a detailed food-symptom journal for at least 6 weeks to identify your personal triggers.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4