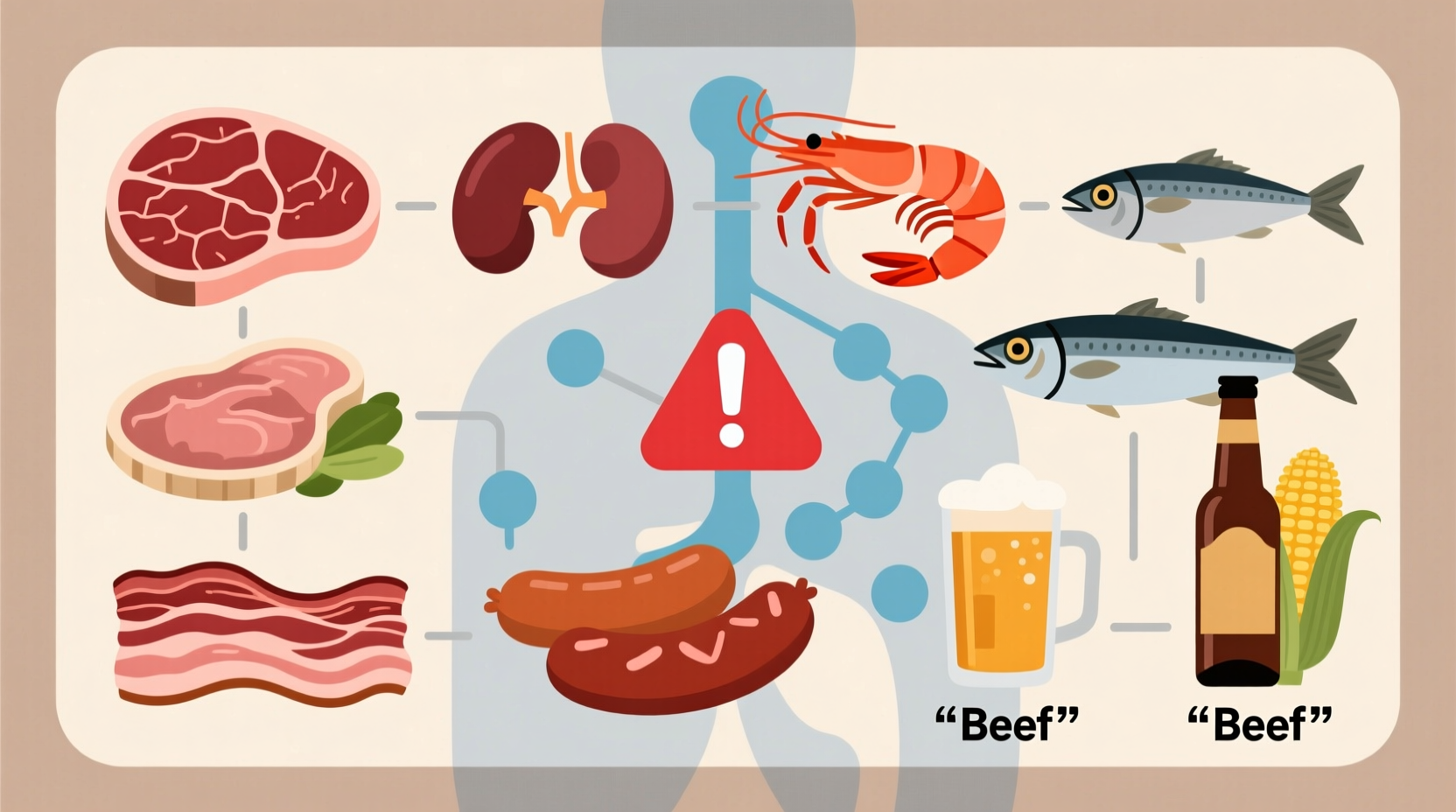
The top foods that aggravate gout include organ meats (liver, kidney), red meats, certain seafood (anchovies, sardines, mussels), sugary drinks with high-fructose corn syrup, and alcoholic beverages—especially beer and spirits. These foods either contain high levels of purines that break down into uric acid or interfere with the body's ability to excrete uric acid, triggering painful gout flare-ups. Understanding which specific foods to limit can significantly reduce symptoms for most gout sufferers.
If you're managing gout, knowing exactly which foods trigger flare-ups isn't just helpful—it's essential for preventing painful joint inflammation. As someone who's experienced the sudden, intense pain of a gout attack, I understand how crucial dietary choices are in controlling this condition. Research shows that strategic food choices can lower uric acid levels by 15-20%, potentially reducing flare-up frequency by nearly half. This guide delivers evidence-based dietary strategies specifically targeting uric acid reduction, so you can make informed decisions at every meal.
Understanding the Gout-Diet Connection
Gout develops when uric acid crystals accumulate in your joints, causing sudden, severe pain—most commonly in the big toe. Uric acid forms when your body breaks down purines, natural compounds found in certain foods and produced by your body. When uric acid levels become too high (hyperuricemia), crystals form in joints, triggering inflammation.
While genetics and kidney function play roles, dietary choices directly impact uric acid production and excretion. The American College of Rheumatology emphasizes that "dietary modification remains a cornerstone of gout management" alongside medication when needed. What you eat doesn't cause gout, but it significantly influences how often and severely you experience symptoms.
Foods That Trigger Gout Flare-Ups: The Complete Breakdown
Not all high-purine foods affect everyone equally, but research consistently identifies specific dietary triggers. Understanding these categories helps you make smarter choices without unnecessary restrictions.
1. Organ Meats and Red Meats: The Highest Risk Foods
Organ meats like liver, kidney, and sweetbreads contain exceptionally high purine levels—up to 5 times more than regular meats. A single 3-ounce serving can contain 400-500 mg of purines, compared to 100-200 mg in lean cuts of beef or pork.
According to the American College of Rheumatology, reducing red meat consumption by just 50% can lower uric acid levels by 0.5-1.0 mg/dL within weeks. This seemingly small change significantly reduces crystal formation risk.
2. Certain Seafood Varieties: Proceed with Caution
While most fish provide heart-healthy omega-3s, specific seafood varieties dramatically increase gout risk:
| High-Risk Seafood | Purine Content (per 3 oz) | Recommended Action |
|---|---|---|
| Anchovies, sardines, mussels | 500-1000 mg | Avoid completely |
| Tuna, trout, scallops | 200-400 mg | Limited to 1 serving/week |
| Salmon, shrimp | 100-200 mg | Moderate consumption (2-3 servings/week) |
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) notes that "shellfish and oily fish contribute significantly to uric acid production" but emphasizes that not all seafood needs elimination—strategic selection matters.
3. Sugary Beverages and Fructose: The Hidden Culprit
Research published in Arthritis & Rheumatism found that men who consumed two or more sugar-sweetened soft drinks daily had an 85% higher risk of developing gout compared to those who drank less than one monthly. High-fructose corn syrup triggers uric acid production through multiple metabolic pathways.
Even fruit juices with concentrated fructose can pose problems. The Arthritis Foundation specifically warns against "fruit juices with added sugar" as significant gout triggers, noting that "whole fruits are generally safe in moderation due to their fiber content."
4. Alcohol: Beer and Spirits Pose Greatest Risk
Alcohol affects gout through two mechanisms: increasing uric acid production and reducing kidney excretion. Beer presents the greatest risk due to both its alcohol content and high purine levels from yeast. A study in The Lancet found that each daily beer increases gout risk by 49%, while spirits increase risk by 15% per drink.
Interestingly, moderate red wine consumption (1-2 glasses) shows minimal impact on uric acid levels according to research from Harvard Medical School, though individual responses vary significantly.

Context Matters: When Diet Alone Isn't Enough
Understanding the boundaries of dietary management is crucial. While diet plays a significant role, the Arthritis Foundation clarifies that "dietary changes alone typically reduce uric acid by only 1-2 mg/dL, whereas medications can lower levels by 3-5 mg/dL." This means:
- Dietary changes work best for mild or infrequent gout
- Those with frequent flare-ups (2+ per year) often need medication
- During acute attacks, medication provides faster relief than dietary changes alone
- Individual responses vary—keep a food journal to identify personal triggers
The Mayo Clinic emphasizes that "successful gout management requires a three-pronged approach: medication when needed, strategic dietary choices, and maintaining a healthy weight." Don't blame yourself if diet alone doesn't control symptoms—gout is a complex metabolic condition.
Practical Implementation: Your 4-Week Action Plan
Changing your diet doesn't need to feel overwhelming. This phased approach helps you implement sustainable changes:
Week 1: Eliminate Highest-Risk Foods
- Remove organ meats completely
- Replace sugary drinks with water or herbal tea
- Limit alcohol to one glass of wine, maximum 2-3 times weekly
Week 2-3: Strategic Substitutions
- Swap red meat for poultry or plant-based proteins
- Choose low-purine fish like salmon over high-risk varieties
- Incorporate cherries (fresh or tart cherry juice) known to reduce uric acid
Week 4: Personalize and Maintain
- Keep a detailed food and symptom journal
- Work with your doctor to monitor uric acid levels
- Gradually reintroduce moderate-risk foods to test tolerance
This approach aligns with recommendations from the Centers for Disease Control and Prevention, which states that "gradual dietary changes are more sustainable and effective than drastic restrictions" for long-term gout management.
What to Eat: Building a Gout-Friendly Plate
Focus on these evidence-backed food groups that may actually help lower uric acid:
- Dairy: Low-fat dairy products reduce gout risk by 43% according to a 12-year Harvard study
- Cherries: Regular consumption lowers flare-up risk by 35% (Arthritis & Rheumatism)
- Whole grains: Replace refined carbs with oats, brown rice, and quinoa
- Plant-based proteins: Tofu, lentils, and beans in moderation
- Plenty of water: Aim for 8-12 glasses daily to help flush uric acid
Remember that individual responses vary significantly. The key is finding your personal tolerance levels while maintaining nutritional balance.
Frequently Asked Questions
Can I ever eat steak if I have gout?
You can enjoy steak occasionally in strict moderation. Limit portions to 3-4 ounces (about the size of a deck of cards) and choose lean cuts like sirloin or tenderloin. Avoid combining steak with other high-purine foods or alcohol. Many gout specialists recommend limiting red meat to 1-2 servings weekly, spacing them at least 3 days apart. Always monitor your body's response and consult your doctor about your specific dietary plan.
Do tomatoes trigger gout attacks?
Recent research suggests tomatoes may trigger gout in some people, though they're not traditionally considered high-purine. A 2014 study in BMC Musculoskeletal Disorders found tomatoes were the fourth most commonly reported dietary trigger after alcohol, red meat, and seafood. If you notice flare-ups after eating tomatoes, consider limiting intake temporarily. However, tomatoes provide valuable nutrients, so complete elimination isn't generally recommended unless you've confirmed they trigger your symptoms.
How quickly can dietary changes reduce gout symptoms?
Dietary changes typically lower uric acid levels within 2-4 weeks, but symptom improvement varies. During an active flare-up, medication provides faster relief than dietary changes alone. For prevention, consistent dietary modifications show significant results in 4-8 weeks. The American College of Rheumatology notes that "sustained dietary changes can reduce flare frequency by 30-50% over 3-6 months" when combined with appropriate medication if needed.
Is coffee bad for gout?
Surprisingly, coffee may actually help reduce gout risk. Multiple studies, including research published in Arthritis & Rheumatism, show that regular coffee consumption (both caffeinated and decaf) is associated with lower uric acid levels and reduced gout incidence. The exact mechanism isn't fully understood, but compounds in coffee may improve insulin sensitivity and kidney function. However, add minimal sugar and avoid excessive consumption (limit to 3-4 cups daily) to prevent other health issues.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4