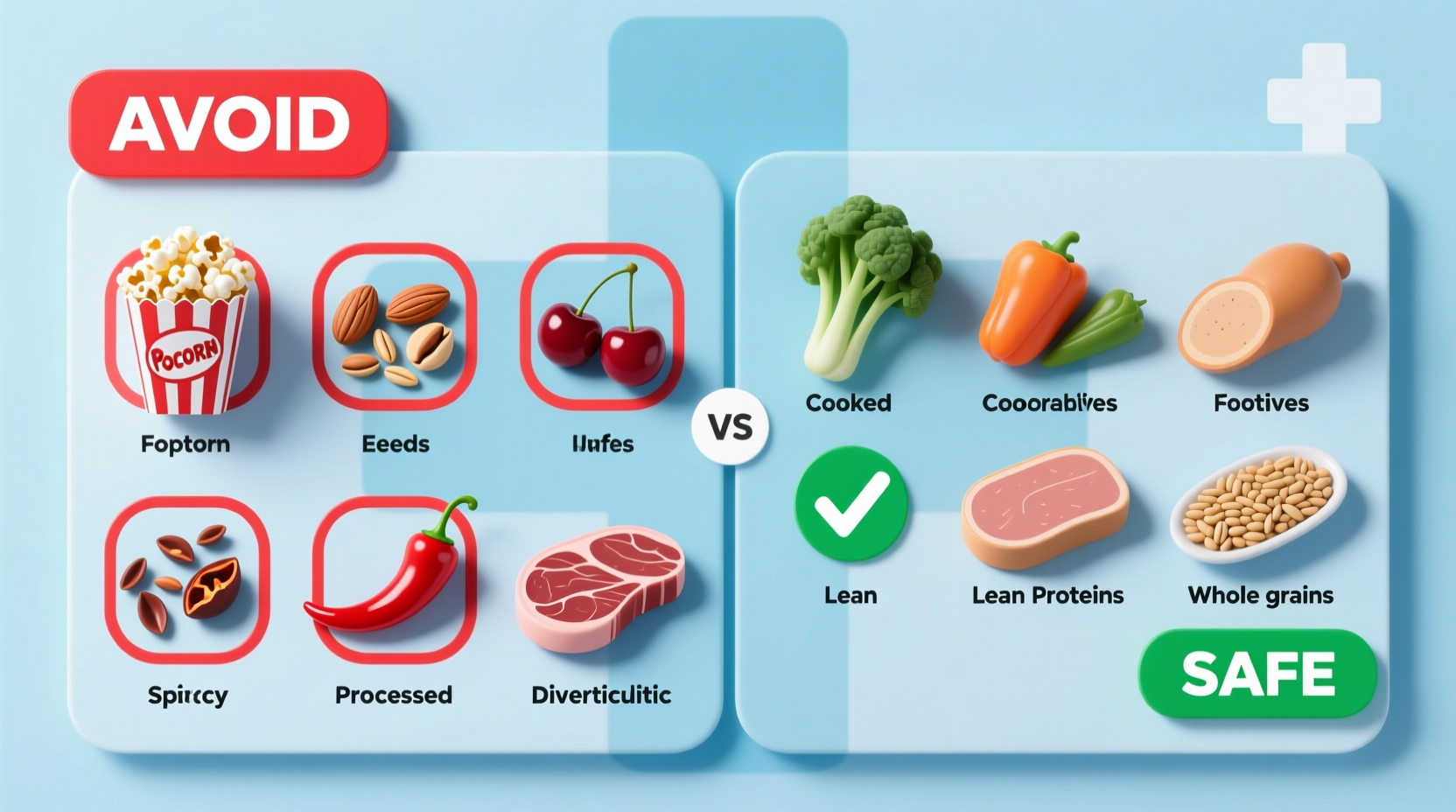
During diverticulitis flare-ups, immediately avoid high-fiber foods, nuts, seeds, popcorn, and hard-to-digest items. Long-term, focus on a high-fiber diet but eliminate personal triggers. Always follow your doctor's specific guidance as individual needs vary.
Your Essential Guide to Diverticulitis Food Restrictions
If you're managing diverticulitis, knowing exactly what food to avoid with diverticulitis could prevent painful flare-ups and support long-term gut health. This evidence-based guide cuts through outdated myths to deliver current medical recommendations from gastroenterology authorities. You'll discover precisely which foods trigger complications during active flare-ups versus long-term maintenance, plus practical alternatives that keep your digestive system calm.
Why Food Choices Matter During Diverticulitis Flare-Ups
When diverticula (small pouches in your colon) become inflamed or infected, your digestive tract needs immediate rest. High-fiber or hard-to-digest foods can aggravate inflammation by increasing pressure and movement in the colon. During acute episodes, medical professionals universally recommend a temporary low-fiber diet to reduce bowel activity while healing occurs. The American College of Gastroenterology emphasizes that improper food choices during flare-ups significantly increase complication risks like abscesses or perforations.
Foods to Avoid During Active Diverticulitis Flare-Ups
During the first 2-3 days of a flare-up, eliminate these high-risk foods completely. These items can worsen inflammation by irritating sensitive colon tissue or requiring excessive digestive effort:
- Whole grains and high-fiber cereals (brown rice, bran flakes, quinoa)
- Raw fruits and vegetables (apples, broccoli, cauliflower)
- Nuts and seeds (almonds, sunflower seeds, chia seeds)
- Popcorn (kernels can lodge in diverticula)
- Beans and legumes (lentils, black beans)
- High-fat fried foods (slows digestion and increases inflammation)
| Food Category | Immediate Flare-Up Avoidance | Long-Term Consideration |
|---|---|---|
| Nuts & Seeds | Avoid completely | Generally safe after recovery (per current guidelines) |
| Popcorn | Strictly prohibited | Limited intake after healing; monitor tolerance |
| Raw Vegetables | Avoid entirely | Gradually reintroduce cooked versions |
| Beans/Legumes | Eliminate | Reintroduce slowly in small portions |
This dietary evolution reflects significant changes in medical understanding. As noted in the American College of Gastroenterology's 2023 guidelines, the historical blanket ban on nuts and seeds has been replaced by individualized recommendations based on newer research showing no increased flare-up risk from these foods in most patients.
Long-Term Dietary Management After Recovery
Once inflammation subsides (typically after 2-4 weeks), gradually transition to a high-fiber diet proven to prevent future flare-ups. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recommends 25-30 grams of daily fiber to maintain colon health. However, certain foods may remain problematic depending on your individual tolerance:
- Personal trigger foods - Common culprits include corn, seeds in tomatoes/cucumbers, and tough meat fibers
- Excessive red meat - Associated with higher recurrence rates per NIH research
- Low-fiber processed foods - White bread, pastries, and refined grains offer no protective benefits
Important context: Dietary needs vary significantly based on disease severity and individual physiology. As the Mayo Clinic explains, "While high-fiber diets benefit most people with diverticular disease, some may require modified approaches if they have strictures or other complications." Always work with your gastroenterologist to develop a personalized plan.
Debunking the Nut and Seed Myth
For decades, patients were told to permanently avoid nuts and seeds due to the unproven theory that particles could lodge in diverticula. Modern research has overturned this advice. A landmark JAMA Internal Medicine study tracking 47,000 men for 18 years found those consuming nuts twice weekly had 20% fewer diverticulitis episodes. Current guidelines from major medical institutions now state:
"There is no evidence supporting the avoidance of nuts, seeds, and popcorn in patients with diverticular disease. These foods may actually provide protective benefits through their fiber and nutrient content." - American Gastroenterological Association

Practical Food Swaps for Immediate Relief
When symptoms strike, these evidence-based substitutions provide nutrition without aggravating your condition:
- Instead of raw apples: Applesauce or baked pears
- Instead of whole wheat bread: White toast or refined grain crackers
- Instead of broccoli: Well-cooked carrots or green beans without skins
- Instead of almonds: Smooth nut butters (in small quantities after initial healing phase)
Transition carefully: Increase fiber by just 5 grams daily after recovery. Sudden increases can trigger new flare-ups. The Cleveland Clinic recommends keeping a detailed food diary to identify your personal triggers during this reintroduction phase.
When to Consult Your Healthcare Team
Dietary management requires professional guidance, especially if you experience:
- Recurrent flare-ups despite dietary changes
- Difficulty maintaining nutrition during restrictions
- Signs of complications (fever, severe pain, vomiting)
Registered dietitians specializing in gastrointestinal disorders can create customized meal plans that balance nutritional needs with symptom prevention. The Academy of Nutrition and Dietetics confirms that personalized nutrition counseling significantly improves outcomes for diverticulitis patients compared to generic advice.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4