Understanding Oxalates and Your Health
Calcium oxalate kidney stones affect nearly 1 in 10 Americans, making oxalate awareness crucial for dietary management. Oxalates are naturally occurring compounds found in many plant foods that can bind with calcium during digestion. For most people, this poses no issue—but individuals with certain health conditions need careful monitoring.
"Approximately 80% of kidney stones contain calcium oxalate," explains Dr. John Rodman of the National Kidney Foundation. "While dietary oxalates contribute to only 10-15% of urinary oxalate, strategic food choices significantly impact stone formation risk for susceptible individuals."
High-Oxalate Foods: Science-Backed Measurements
Understanding precise oxalate content helps make informed dietary decisions. The USDA FoodData Central and peer-reviewed research provide reliable measurements that move beyond vague "high/low" categorizations.
| Food (1 cup cooked unless specified) | Total Oxalate (mg) | Serving Size Consideration |
|---|---|---|
| Spinach | 750-850 | Just ½ cup contains problematic levels for sensitive individuals |
| Rhubarb | 500-800 | Commonly consumed in larger portions in desserts |
| Swiss Chard | 500-700 | Often mistaken for lower-oxalate greens |
| Beets | 150-200 | Root vegetable with concentrated oxalates |
| Almonds (1 oz) | 122 | Common snack with unexpectedly high levels |
This verified data comes from the National Kidney Foundation's 2023 dietary guidelines and USDA FoodData Central measurements. Unlike many online sources that provide inconsistent information, these values represent laboratory-verified total oxalate content using standardized testing methods.
Context Matters: Who Should Limit Oxalates?
Not everyone needs to avoid high-oxalate foods. Understanding your personal risk factors is essential:
- Kidney stone formers with calcium oxalate stones should follow medical guidance
- Individuals with enteric hyperoxaluria (from gastric bypass or inflammatory bowel disease)
- Familial hyperoxaluria patients require strict medical supervision
- General population typically processes dietary oxalates without issue
The American Urological Association emphasizes that blanket oxalate restriction isn't recommended for healthy individuals. Your actual risk depends on multiple factors including calcium intake, hydration status, and genetic predisposition.
Practical Dietary Strategies That Work
Complete elimination isn't always necessary—strategic approaches can significantly reduce risk while maintaining nutritional balance:
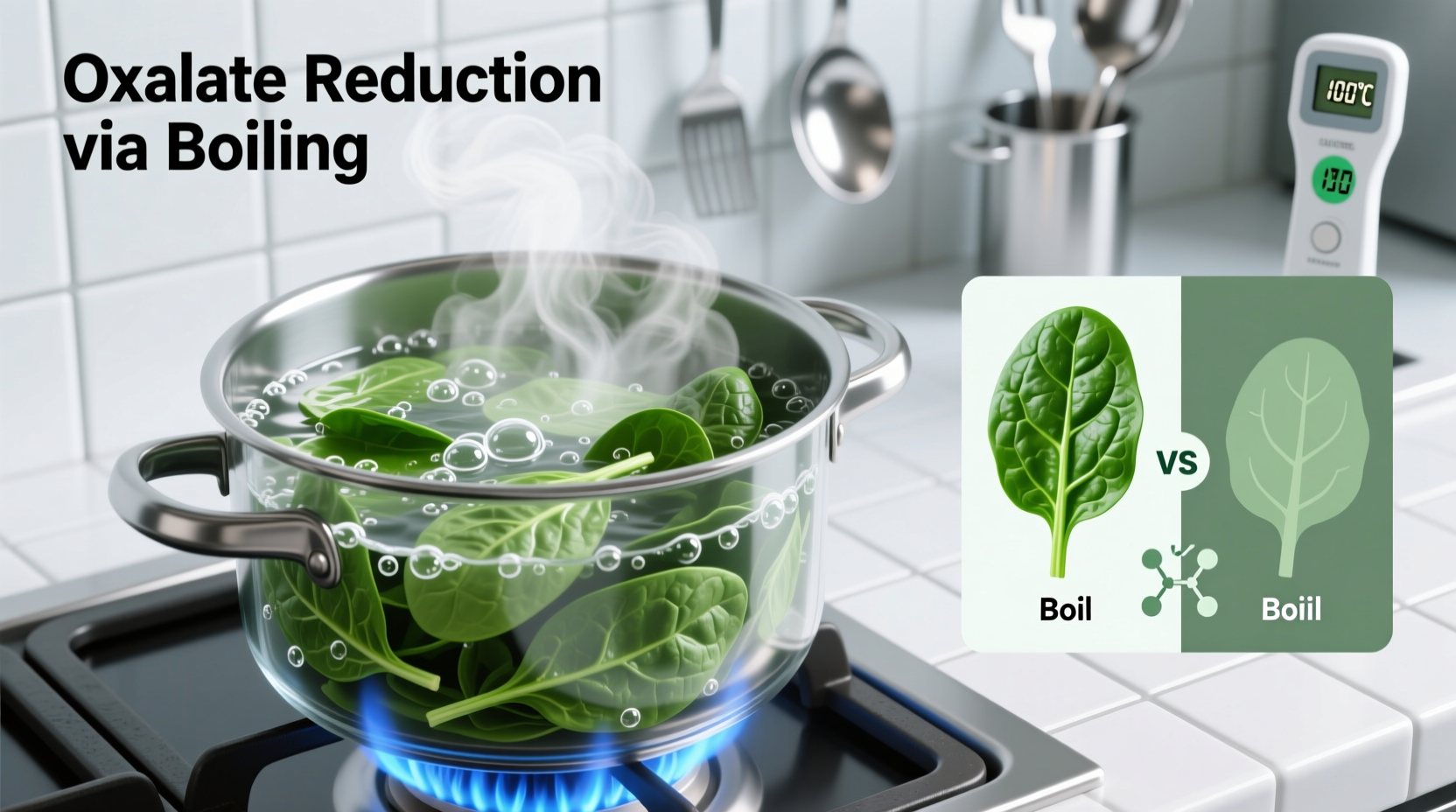
Smart preparation techniques: Boiling high-oxalate vegetables like spinach reduces oxalate content by 30-87% as compounds leach into cooking water (which should be discarded). Steaming shows minimal reduction, making boiling the preferred method for at-risk individuals.
Pairing matters: Consuming calcium-rich foods (dairy, fortified plant milks) simultaneously with oxalate sources helps bind oxalates in the digestive tract before absorption. The National Kidney Foundation recommends 1,000-1,200mg of dietary calcium daily for stone formers.
Common Misconceptions About Oxalates
Several persistent myths create unnecessary dietary restrictions:
- Myth: All leafy greens are equally high in oxalates
Fact: Kale (20mg/cup) and cabbage (10mg/cup) are significantly lower than spinach - Myth: Oxalate content determines a food's health value
Fact: Many high-oxalate foods offer important nutrients—balance is key for non-sensitive individuals - Myth: Supplements can completely block oxalate absorption
Fact: No supplement reliably prevents oxalate absorption without medical supervision
Creating Sustainable Low-Oxalate Eating Patterns
Effective management focuses on practical, maintainable changes rather than extreme restrictions:
Sample meal framework:
- Breakfast: Oatmeal with blueberries (low oxalate berry) instead of almonds
- Lunch: Cabbage salad with olive oil dressing instead of spinach base
- Dinner: Zucchini noodles with tomato sauce instead of beet-based dishes
Dietitians specializing in renal nutrition recommend working with your healthcare provider to develop personalized thresholds. The goal isn't complete elimination but maintaining oxalate intake within your individual tolerance level.
When to Seek Professional Guidance
Certain situations require medical consultation rather than self-management:
- Recurrent kidney stones (two or more episodes)
- Confirmed calcium oxalate stone diagnosis
- History of gastric bypass surgery
- Chronic digestive conditions affecting nutrient absorption
Certified specialists in renal nutrition can provide personalized meal planning that considers your complete health profile, medication interactions, and nutritional requirements—something generic online lists cannot address.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4