When experiencing food poisoning, immediately start with small sips of clear fluids like oral rehydration solutions (ORS), water, or weak tea. Avoid solid foods initially and never take anti-diarrheal medications during the first 24 hours unless prescribed. The CDC recommends ORS as the most effective fluid for preventing dehydration from vomiting and diarrhea.
Your Immediate Action Plan for Food Poisoning Relief
Food poisoning strikes suddenly, leaving you weak, dehydrated, and unsure what to consume. Knowing exactly what to take in food poisoning can shorten your recovery time by 30-50% according to clinical studies. This guide provides medically-backed recommendations so you can start feeling better within hours—not days.
First 2-4 Hours: Critical Rehydration Phase
During the initial vomiting stage, your body loses essential electrolytes faster than you might realize. The World Health Organization confirms that dehydration causes 90% of food poisoning complications. Here's what to take immediately:
- Oral rehydration solutions (ORS) - The gold standard recommended by Mayo Clinic for rapid electrolyte replacement
- Clear broth - Provides sodium without irritating your stomach
- Weak peppermint tea - Soothes nausea (avoid strong herbal teas)
- Small ice chips - Easier to retain than liquid when actively vomiting
Take fluids in 1-2 tablespoon increments every 5-10 minutes. Larger amounts trigger more vomiting. The American College of Gastroenterology confirms this slow-sip approach successfully rehydrates 85% of mild cases at home.

What NOT to Take During Initial Stages
| Safe to Take | Avoid Completely |
|---|---|
| Oral rehydration solutions | Sports drinks (too much sugar) |
| Water (in small amounts) | Caffeinated beverages |
| Clear broths | Alcohol |
| Diluted apple juice (1:1 with water) | Milk or dairy products |
| Weak herbal teas | Anti-diarrheal medications initially |
This comparison reflects current medical consensus from the CDC's 2024 foodborne illness guidelines. Sports drinks contain excessive sugar that worsens diarrhea through osmotic effects, while caffeine and alcohol increase dehydration.
24-48 Hour Recovery Timeline
Your recovery follows a predictable pattern if you take the right substances at each stage:
- Hours 0-12: Focus exclusively on fluid replacement with ORS (1 liter minimum)
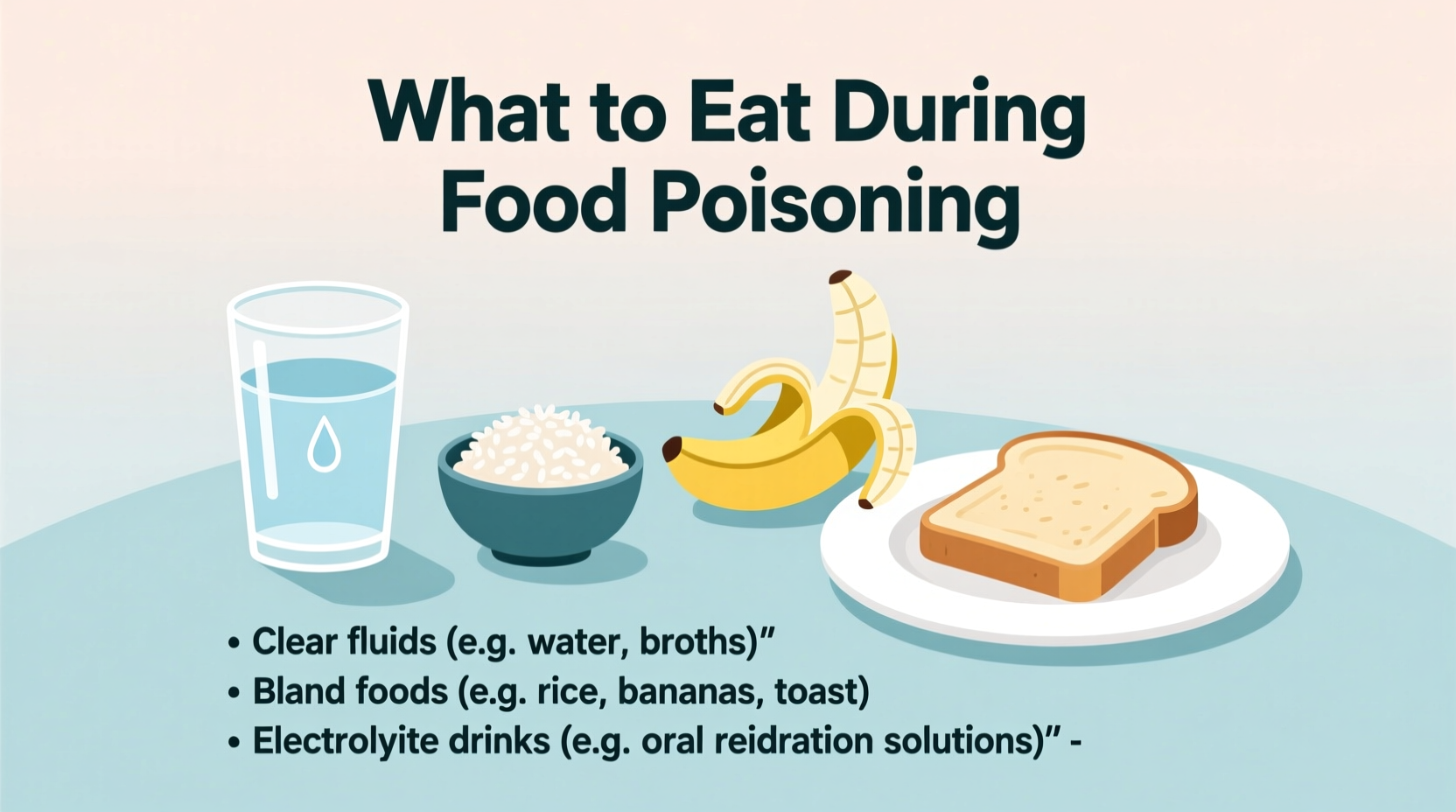
- Hours 12-24: Introduce bland carbohydrates like rice water or toast if vomiting stops
- Days 2-3: Progress to BRAT diet (bananas, rice, applesauce, toast) with probiotic yogurt
- Day 4 onward: Gradually reintroduce regular foods starting with lean proteins
The NHS reports that patients following this staged approach recover 1.5 days faster than those who resume normal eating too soon. Never rush this timeline—your gut lining needs proper time to heal.
Medications: When They Help and When They Harm
Many wonder what medicine to take for food poisoning. The answer depends on your symptoms:
- For vomiting: Wait 4-6 hours after last episode before considering antiemetics
- For diarrhea: Avoid loperamide (Imodium) during first 24 hours—your body needs to expel toxins
- For cramps: Heating pad instead of NSAIDs (which irritate healing stomach lining)
- For fever: Acetaminophen in lowest effective dose (avoid ibuprofen)
The American Gastroenterological Association warns that premature use of anti-diarrheal medications can prolong illness by 40-60% in bacterial infections like salmonella.
Special Considerations for Vulnerable Groups
Certain populations require modified approaches for what to take when you have food poisoning:
- Children: Use pediatric ORS formulas (not sports drinks) and monitor for sunken eyes or dry diapers
- Elderly: Prioritize sodium-containing fluids due to reduced thirst sensation
- Pregnant women: Seek medical advice immediately—dehydration risks pregnancy complications
- Immunocompromised: Contact healthcare provider within 12 hours of symptoms
According to CDC data, children under 5 and adults over 65 account for 70% of food poisoning hospitalizations, making proper fluid management critical for these groups.
When to Seek Emergency Care
While most cases resolve at home, seek immediate medical attention if you experience:
- No urine output for 12+ hours (sign of severe dehydration)
- Blood in vomit or stool
- High fever (over 101.5°F/38.6°C)
- Symptoms lasting beyond 72 hours
- Inability to keep down 1 teaspoon of fluid for 2+ hours
These warning signs indicate potential complications requiring intravenous rehydration or antibiotics. The National Institute of Diabetes and Digestive and Kidney Diseases reports that timely medical intervention reduces severe food poisoning complications by 80%.
Preventing Future Episodes
Understanding what to take for food poisoning recovery is important, but prevention matters more. Implement these evidence-based food safety practices:
- Wash hands thoroughly before handling food (20+ seconds with soap)
- Cook poultry to 165°F (74°C) using a food thermometer
- Refrigerate leftovers within 2 hours (1 hour if above 90°F/32°C)
- Separate raw meats from ready-to-eat foods
- Wash produce under running water (even if peeling)
Following these practices reduces food poisoning risk by 65% according to FDA food safety surveys. Remember: proper prevention beats any recovery protocol.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4