Immediate Actions During Food Poisoning
When food poisoning strikes, your first 24 hours determine recovery speed. The Centers for Disease Control and Prevention (CDC) reports that nearly 48 million Americans experience foodborne illnesses annually. Your immediate response matters more than you think.
Stop consuming solid foods for the first 6-8 hours while your stomach settles. Instead, take small sips of clear fluids every 5-10 minutes. Oral rehydration solutions (like WHO-recommended formulas) work better than plain water because they contain the precise electrolyte balance your body needs. The World Health Organization confirms these solutions reduce dehydration-related complications by 70% compared to water alone.
First 24-Hour Timeline: What to Expect
| Timeframe | Physical Response | Action Required |
|---|---|---|
| 0-6 hours | Nausea intensifies, possible vomiting begins | Rest lying on side, take tiny sips of fluid |
| 6-12 hours | Diarrhea typically starts, cramping increases | Maintain fluid intake, avoid anti-diarrheals |
| 12-24 hours | Peak symptoms, possible dehydration signs | Monitor urine color, continue electrolytes |
| 24+ hours | Symptoms gradually improve | Introduce BRAT diet (bananas, rice, applesauce, toast) |
When to Seek Emergency Medical Care
Knowing critical warning signs separates manageable cases from dangerous situations. According to Mayo Clinic guidelines, seek immediate medical attention if you experience:
- Bloody or black stools indicating possible gastrointestinal bleeding
- Fever exceeding 102°F (38.9°C) suggesting bacterial infection
- Signs of severe dehydration: minimal urine output for 12+ hours, dizziness when standing, or rapid heartbeat
- Vomiting that prevents keeping any liquids down for more than 12 consecutive hours
- Numbness, blurred vision, or muscle weakness which may indicate botulism
High-risk groups including infants, elderly adults, pregnant women, and immunocompromised individuals should contact healthcare providers at the first sign of food poisoning. The CDC emphasizes that certain pathogens like listeria require prompt antibiotic treatment.
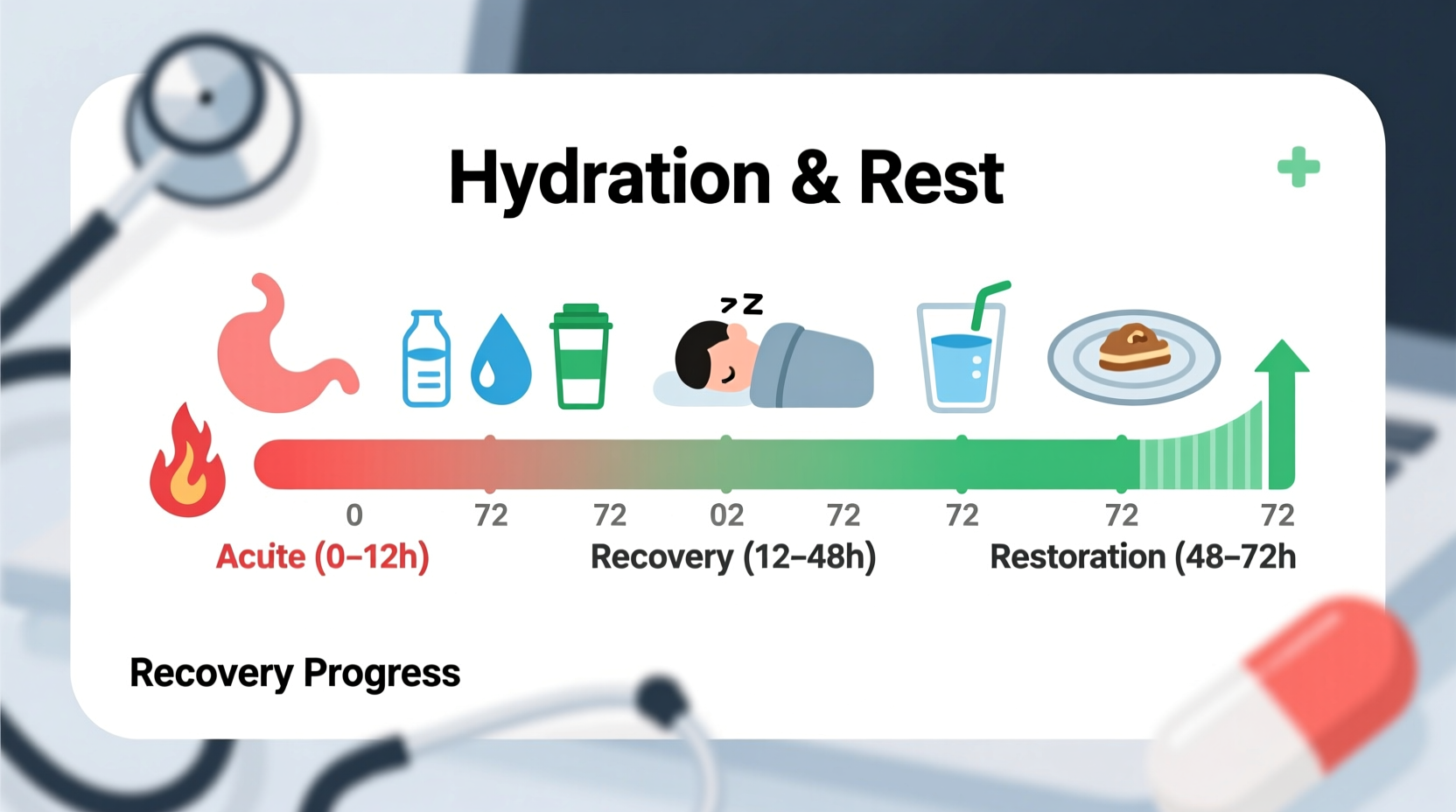
Hydration Strategy That Actually Works
Proper hydration isn't just about drinking more—it's about drinking smart. Most people make the mistake of consuming large amounts of water at once, which often triggers more vomiting. Instead, follow this medically-approved approach:
- Start with 1-2 teaspoons of fluid every 5 minutes for the first hour
- Gradually increase to 1-2 tablespoons every 5-10 minutes as tolerated
- Use oral rehydration solutions containing 6% glucose and precise sodium/potassium ratios
- Avoid sugary drinks, caffeine, and dairy which worsen symptoms
The NHS recommends monitoring hydration through urine color—aim for pale yellow, not dark amber. Dark urine after 12 hours of fluid intake indicates worsening dehydration requiring medical evaluation.
Recovery Diet Progression Plan
Reintroducing food requires strategic timing. Jumping to solid foods too soon prolongs recovery. Follow this evidence-based progression:
- Days 1-2: Clear liquids only (broth, oral rehydration solutions, weak tea)
- Days 2-3: Bland carbohydrates (white rice, plain toast, bananas)
- Days 3-5: Soft proteins (scrambled eggs, boiled chicken)
- Days 5-7: Gradual return to normal diet
Avoid these common recovery mistakes:
- Consuming spicy or fatty foods too soon
- Using anti-diarrheal medications during initial phase (traps pathogens)
- Returning to normal eating before symptoms fully resolve
Preventing Future Episodes
Food safety practices significantly reduce recurrence risk. Implement these CDC-recommended habits:
- Wash hands thoroughly before handling food and after bathroom use
- Cook meats to proper internal temperatures (use a food thermometer)
- Refrigerate leftovers within 2 hours (1 hour if temperature exceeds 90°F/32°C)
- Separate raw meats from ready-to-eat foods during storage and preparation
Remember that food poisoning often results from multiple contamination points. The FDA reports that improper temperature control causes nearly 40% of foodborne illness cases. When dining out, trust your instincts about questionable food safety practices.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4