Understanding Migraine Food Triggers: Science Over Speculation
When you're searching for what foods trigger migraines, you need reliable information that separates scientific evidence from anecdotal claims. Migraines affect approximately 12% of the population, and for many sufferers, certain foods can trigger or worsen attacks. However, identifying your personal triggers requires understanding both the established science and your unique physiology.
Unlike popular myths that suggest "everyone" should avoid specific foods, research shows significant individual variation in food triggers. The American Migraine Foundation confirms that while certain foods are commonly reported triggers, not everyone reacts to the same substances. This is why a personalized approach beats generic "avoid these 10 foods" lists.
The Science Behind Food-Triggered Migraines
Migraines involve complex neurological processes where certain food compounds can influence blood vessels, neurotransmitters, and inflammation pathways. Key mechanisms include:
- Tyramine - Found in aged foods, this compound affects blood pressure regulation
- Phenylethylamine - Can influence serotonin levels in the brain
- Nitrites and nitrates - Cause blood vessel dilation in sensitive individuals
- MSG and aspartame - May affect glutamate pathways in the nervous system
According to the National Institute of Neurological Disorders and Stroke (NINDS), these compounds don't cause migraines in everyone but can lower the threshold for attacks in susceptible individuals when combined with other factors like stress or hormonal changes.
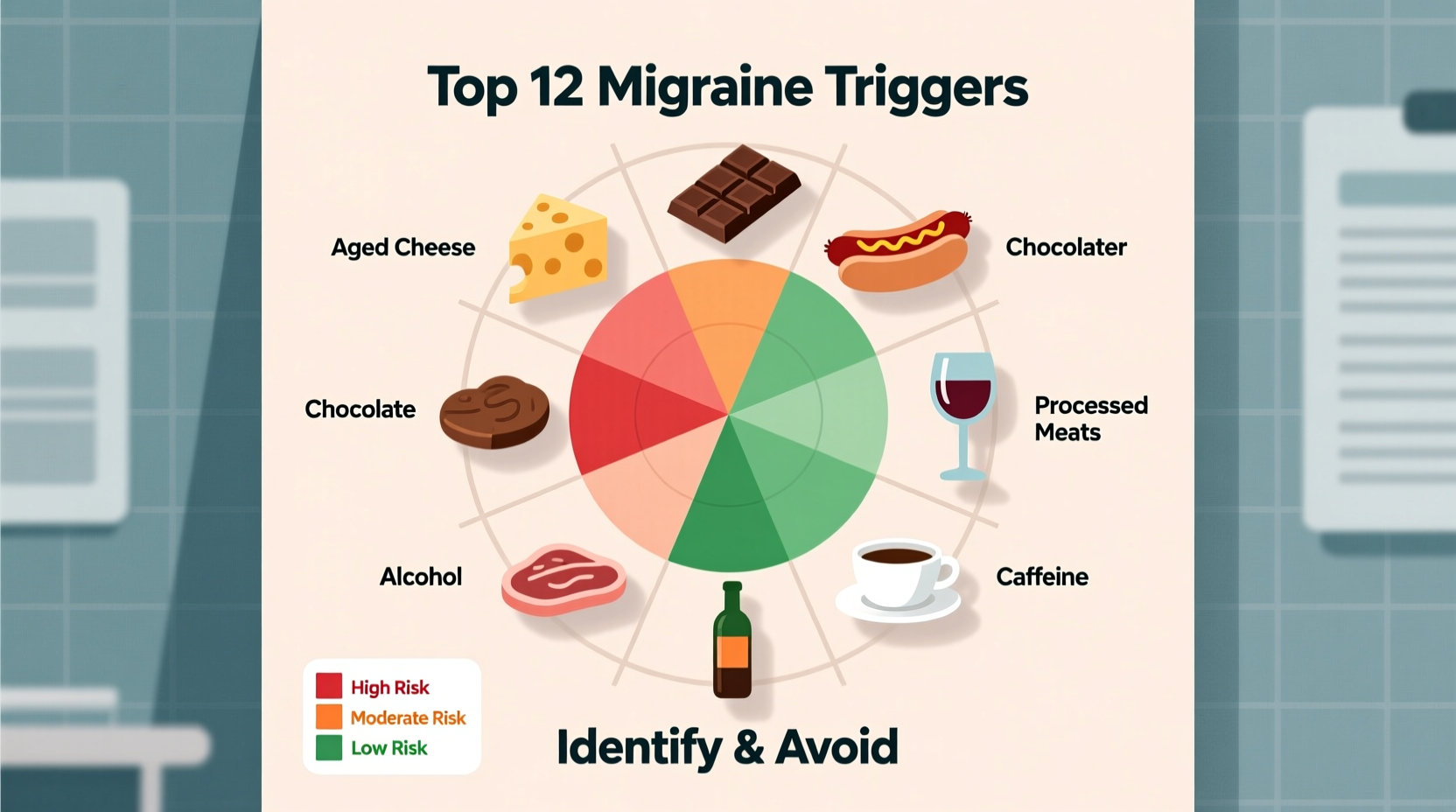
Evidence-Based Migraine Trigger Foods: What Research Shows
Not all "trigger food" claims have equal scientific support. This fact comparison table separates well-documented triggers from less certain associations based on current research:
| Strong Evidence Triggers | Possible Triggers (Individual Variation) | Minimal Evidence |
|---|---|---|
| Aged cheeses (cheddar, blue, parmesan) | Citrus fruits (for some individuals) | All dairy products |
| Red wine and alcohol (histamine content) | Yogurt and fresh cheeses | Most fresh fruits |
| Processed meats (nitrates/nitrites) | Chocolate (for some people) | Whole grains |
| Monosodium glutamate (MSG) | Nuts (especially peanuts) | Most vegetables |
| Artificial sweeteners (aspartame) | Caffeine (both excess and withdrawal) | Seafood (except smoked) |
Source: American Migraine Foundation, Mayo Clinic, and Journal of Headache and Pain (2023)
Why Your Triggers Might Differ From Others
Understanding migraine food triggers by individual is crucial. Research published in Cephalalgia shows that food triggers rarely act alone—they typically combine with other factors like:
- Sleep patterns (both deprivation and excess)
- Hormonal fluctuations
- Stress levels
- Environmental factors
- Hydration status
This explains why you might tolerate a trigger food on a good day but experience a migraine when multiple factors align. The American Migraine Foundation emphasizes that "the same food may trigger a migraine in one person but not another, and may trigger a migraine at one time but not another for the same person."
Your Step-by-Step Guide to Identifying Personal Triggers
Instead of eliminating multiple foods at once, follow this evidence-based approach to identify your specific food triggers for migraine prevention:
- Keep a detailed food and symptom diary for at least 6-8 weeks, noting not just what you eat but timing, stress levels, sleep quality, and menstrual cycle (if applicable)
- Focus on patterns, not single incidents - migraines often result from multiple triggers combining
- Implement a structured elimination diet under healthcare guidance, removing one potential trigger at a time
- Reintroduce foods systematically with 3-5 day intervals between testing
- Consider professional testing for food sensitivities if self-tracking proves difficult
The Mayo Clinic recommends this method over broad elimination diets, which can lead to unnecessary dietary restrictions and potential nutrient deficiencies.
Practical Dietary Strategies for Migraine Management
Once you've identified potential triggers, implement these practical strategies:
- Read labels carefully - nitrates appear in unexpected products, and MSG hides under many names
- Choose fresh over processed - most trigger compounds develop during aging or processing
- Stay hydrated - dehydration is a common migraine trigger that compounds food effects
- Maintain regular meal timing - skipping meals can trigger migraines independently
- Consider cooking methods - grilling can create additional trigger compounds not present in raw ingredients
Remember that complete elimination isn't always necessary—many people can tolerate small amounts of trigger foods. The key is understanding your personal threshold, which may change over time as your body's sensitivity shifts.
When to Seek Professional Guidance
While dietary changes can help manage migraines, consult a healthcare provider if:
- You experience more than 2 migraines per month
- Your symptoms worsen despite dietary changes
- You need guidance on safe elimination diets
- You're considering supplements for migraine prevention
A registered dietitian specializing in headache disorders can help you create a balanced elimination diet that maintains nutritional adequacy while identifying triggers. The National Headache Foundation maintains a provider directory to help you find specialists in your area.
Common Questions About Migraine Food Triggers
How long after eating a trigger food does a migraine typically occur?
The timing varies significantly between individuals. For most people, migraines develop within 12-24 hours after consuming a trigger food, though some experience symptoms within 2-6 hours. The American Migraine Foundation notes that chocolate triggers may take 30 minutes to 2 hours, while aged cheese reactions often occur 6-12 hours later. Keeping a detailed food diary helps identify your personal reaction timeline.
Can I still drink coffee if I have migraines?
Caffeine has a dual relationship with migraines. Small, consistent amounts may help prevent migraines for some people, but both excessive consumption and withdrawal can trigger attacks. The key is consistency—sudden changes in your caffeine intake are more problematic than moderate daily consumption. If you're sensitive, limit yourself to one consistent serving per day and avoid abrupt changes to your routine.
Why do some people get migraines from red wine but not white wine?
Red wine contains higher levels of histamine and tyramine than white wine, along with additional compounds from grape skins and seeds used in red wine production. These substances can trigger migraines in susceptible individuals. However, some people react to white wine as well, particularly if it contains sulfites or other additives. Individual sensitivity varies significantly, so personal tracking is essential rather than blanket avoidance.
Are there foods that can help prevent migraines?
While research is ongoing, certain foods may help reduce migraine frequency for some people. Magnesium-rich foods like leafy greens, nuts, and seeds show promise in studies. Omega-3 fatty acids from fatty fish may reduce inflammation. Staying hydrated with water and maintaining stable blood sugar with regular meals containing complex carbohydrates also supports migraine prevention. However, no single "miracle food" works for everyone—focus on overall dietary patterns rather than quick fixes.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4