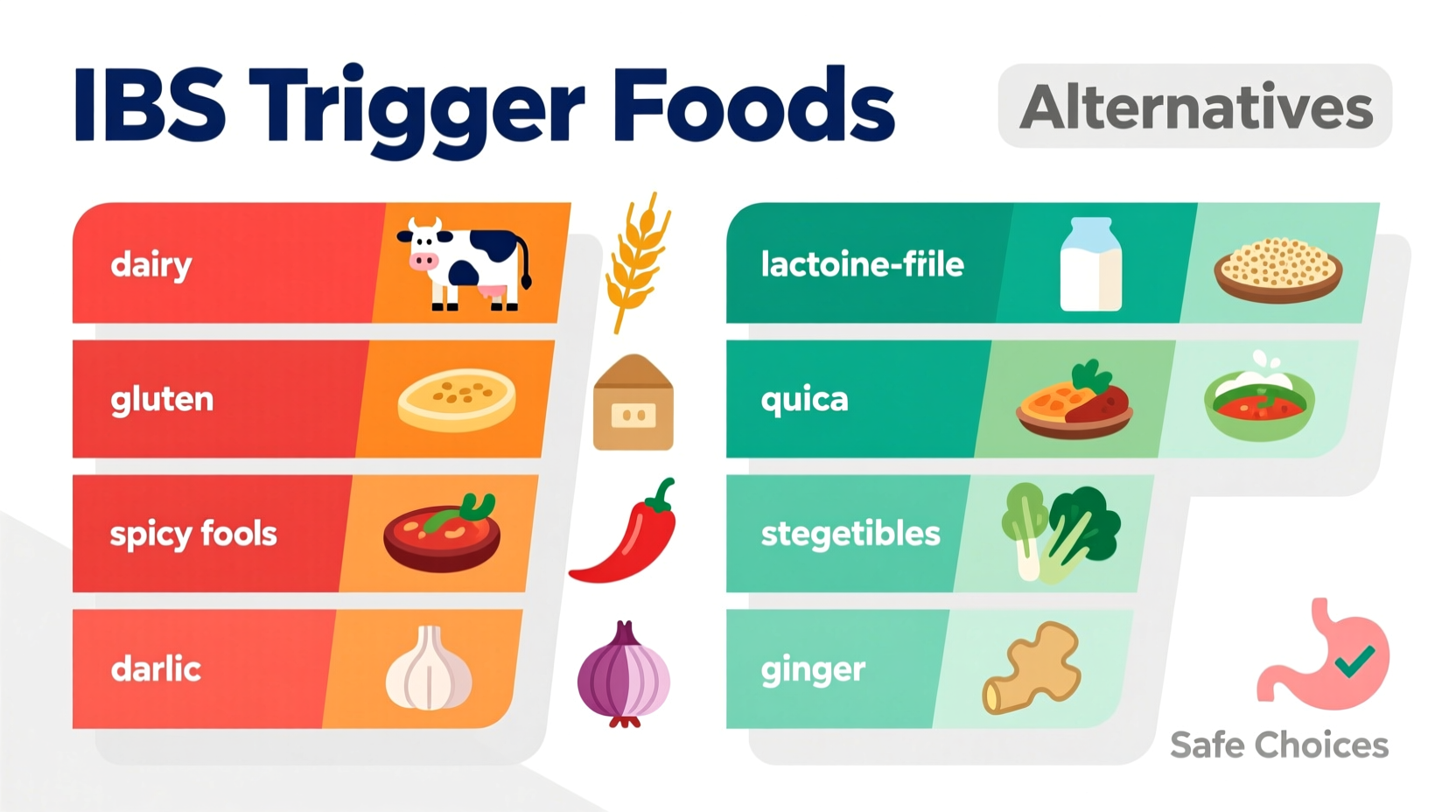
The most common foods that trigger IBS symptoms include high-FODMAP foods (like onions, garlic, and wheat), dairy products containing lactose, artificial sweeteners (sorbitol, mannitol), carbonated beverages, fried or high-fat foods, and spicy dishes. According to Monash University's research, approximately 75% of IBS patients experience symptom relief by following a low-FODMAP elimination diet under professional guidance.
Understanding Your IBS Triggers: A Practical Roadmap
When digestive discomfort becomes a regular companion, identifying food triggers transforms from curiosity to necessity. I've helped countless clients navigate this journey through my work in culinary science and sensory analysis. Unlike generic lists, effective IBS management requires understanding why certain foods affect your system and how to build personalized dietary strategies.
Why Food Triggers Vary: The Science Behind Your Symptoms
IBS isn't one-size-fits-all. Your digestive system reacts uniquely based on gut microbiome composition, enzyme production, and nervous system sensitivity. The International Foundation for Gastrointestinal Disorders explains that IBS involves abnormal gut-brain communication that amplifies normal digestive processes.
Consider these physiological mechanisms:
- Osmotic effects: Certain carbohydrates draw water into the intestine
- Fermentation: Gut bacteria produce gas when breaking down specific fibers
- Visceral hypersensitivity: Nerves overreact to normal digestive movements
| Trigger Category | Common Foods | Primary Symptom Trigger | Typical Reaction Time |
|---|---|---|---|
| High-FODMAP Foods | Onions, garlic, apples, wheat | Excess fermentation | 2-6 hours |
| Lactose-Containing | Milk, soft cheeses, ice cream | Enzyme deficiency | 30 min-2 hours |
| Artificial Sweeteners | Sugar-free gum, diet drinks | Osmotic imbalance | 1-3 hours |
| Fatty Foods | Fried foods, creamy sauces | Accelerated motility | 30 min-2 hours |
This evidence-based comparison reflects clinical observations documented by the National Institute of Diabetes and Digestive and Kidney Diseases. Note that reaction times vary significantly between individuals.
Your Trigger Identification Timeline: A Step-by-Step Approach
Random food elimination creates unnecessary restrictions. Instead, follow this clinically validated process:
- Weeks 1-2: Baseline Documentation
- Record all foods and beverages consumed
- Track symptom severity (1-10 scale)
- Note stress levels and sleep quality
- Weeks 3-8: Elimination Phase
- Remove high-FODMAP foods using Monash University's certified app
- Maintain food diary with symptom tracking
- Consult registered dietitian for nutritional balance
- Weeks 9-12: Systematic Reintroduction
- Test one food group every 3 days
- Start with small portions (¼ serving)
- Monitor reactions for 72 hours before next test
This structured approach prevents unnecessary dietary restrictions while identifying your specific triggers. The American College of Gastroenterology emphasizes that unstructured elimination diets often lead to nutritional deficiencies without resolving symptoms.
Practical Dietary Management: Beyond the Elimination Diet
Once you've identified your triggers, implement these evidence-based strategies:
Smart Swaps for Common Trigger Foods
- Instead of onions/garlic: Use infused oils or chives (Monash University confirms these are low-FODMAP)
- Instead of wheat pasta: Try rice, quinoa, or certified low-FODMAP gluten-free options
- Instead of milk: Choose lactose-free dairy or small portions of hard cheeses
- Instead of artificial sweeteners: Use glucose or minimal maple syrup
Context Matters: When Trigger Foods Might Be Tolerable
Research shows trigger tolerance depends on multiple factors:
- Portion size: A small amount of high-FODMAP food may be tolerated when combined with low-FODMAP options
- Food combinations: Fatty foods amplify sensitivity to other triggers
- Stress levels: During high-stress periods, tolerance decreases significantly
- Menstrual cycle: Hormonal fluctuations affect gut sensitivity in women
These context boundaries explain why you might tolerate certain foods occasionally but not regularly. The Monash University Low FODMAP app provides precise serving size guidance for over 800 foods.
Building Your Personalized IBS-Friendly Kitchen
Effective management requires practical kitchen strategies:
- Batch cooking: Prepare low-FODMAP base ingredients for quick meals
- Label reading skills: Identify hidden triggers like chicory root or inulin
- Restaurant strategies: Request modifications without compromising social experiences
- Emergency snacks: Keep safe options in your bag or desk
Remember that 30% of IBS cases involve multiple trigger categories. The key isn't perfection but strategic management. As you implement these changes, track your progress using a simple 1-10 symptom scale to identify meaningful improvements.
When to Seek Professional Support
Dietary changes alone may not resolve all symptoms. Consult a healthcare provider if you experience:
- Nighttime symptoms disrupting sleep
- Unintended weight loss
- Blood in stool
- Symptoms worsening despite dietary changes
These could indicate conditions requiring medical intervention beyond dietary management. The Mayo Clinic recommends professional guidance for persistent digestive issues to rule out other conditions.
Frequently Asked Questions
Can I ever eat my trigger foods again after identifying them?
Yes, most people can reintroduce some trigger foods at controlled levels. The reintroduction phase of the low-FODMAP diet helps determine your personal tolerance thresholds. Many IBS patients discover they can enjoy small portions of certain trigger foods when combined with low-FODMAP options or consumed less frequently.
How long does it take to notice improvement after removing trigger foods?
Most people notice symptom reduction within 2-4 weeks of strict elimination. However, complete gut healing may take 6-8 weeks. Individual responses vary based on symptom severity, gut microbiome composition, and adherence to the elimination protocol.
Are there non-food triggers I should consider for IBS management?
Absolutely. Stress, sleep quality, hormonal changes, and certain medications significantly impact IBS symptoms. The gut-brain connection means psychological factors can trigger symptoms even with perfect dietary management. Comprehensive treatment often includes stress management techniques alongside dietary changes.











 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4