For those managing diverticulitis, understanding which foods trigger symptoms is crucial for preventing painful flare-ups and supporting digestive health. This guide delivers evidence-based dietary recommendations from leading gastroenterology authorities, helping you make informed choices that align with current medical understanding—not outdated myths.
The Evolution of Diverticulitis Dietary Guidance
Medical understanding of diverticulitis nutrition has significantly evolved over the past two decades. Historically, doctors universally recommended avoiding all seeds, nuts, and popcorn due to the theoretical risk of these foods lodging in diverticula pouches. However, modern research has largely debunked this assumption.
| Time Period | Common Dietary Recommendations | Current Validity |
|---|---|---|
| 1980s-2000s | Avoid all seeds, nuts, corn, and popcorn | Mostly outdated |
| 2000s-2010s | Restrict only during acute flare-ups | Partially valid |
| 2010s-Present | Personalized approach based on individual tolerance | Current standard |
According to research published in the American Journal of Gastroenterology, there's no scientific evidence that seeds and nuts cause diverticulitis complications. In fact, populations with high nut and seed consumption often show lower rates of diverticular disease. This paradigm shift reflects improved understanding of how dietary fiber actually protects against complications.
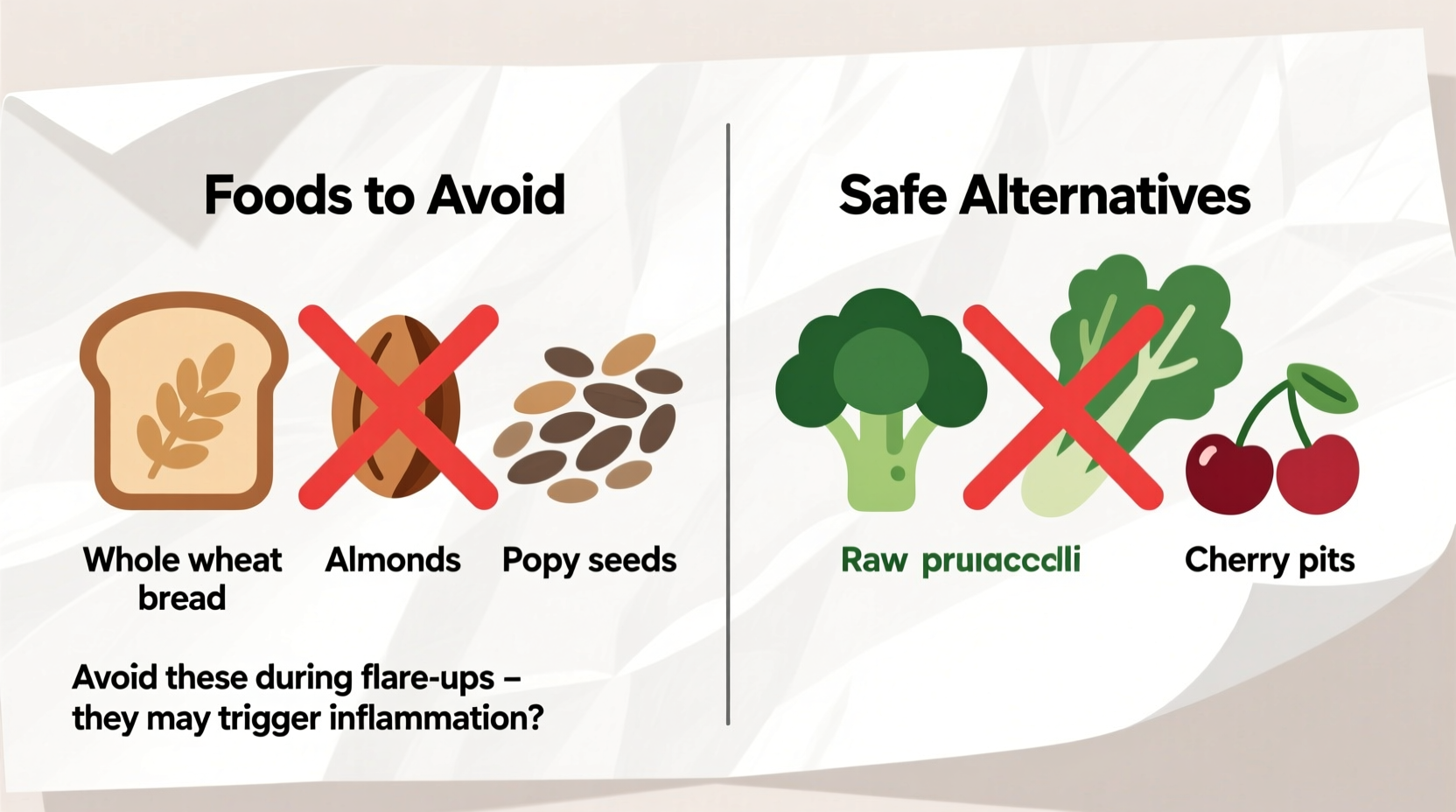
Foods to Avoid During Acute Flare-Ups
When experiencing active diverticulitis symptoms—fever, abdominal pain, and changes in bowel habits—your digestive system needs rest. During these critical periods, follow these evidence-based restrictions:
- Low-residue diet requirements: For 2-4 days during severe flare-ups, your doctor may recommend a clear liquid or full liquid diet before transitioning to low-fiber foods
- Foods that increase digestive workload: Whole grains, raw vegetables, and high-fiber fruits
- Gas-producing foods: Beans, lentils, carbonated beverages, and cruciferous vegetables like broccoli
- Spicy foods: Hot peppers and heavily spiced dishes that may irritate inflamed tissue
During acute episodes, focus on easily digestible options like white rice, cooked carrots, applesauce, and lean proteins. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) emphasizes that this temporary dietary shift helps reduce intestinal pressure while inflammation subsides.
Long-Term Dietary Considerations
Once symptoms improve, gradually reintroduce fiber under medical guidance. Contrary to previous recommendations, current guidelines from the American Gastroenterological Association actually encourage moderate nut and seed consumption for long-term management.

However, certain foods may trigger individual sensitivities. Keep a food diary to identify your personal triggers, which commonly include:
- Popcorn kernels: While research doesn't support avoiding all seeds, the hard, irregular shape of popcorn kernels may irritate some individuals
- Unripe bananas: High in resistant starch that can cause bloating
- Raw vegetables with tough skins: Such as bell peppers and eggplant
- High-FODMAP foods: For those with concurrent IBS symptoms
Context-Specific Dietary Recommendations
Your dietary needs vary significantly based on your current health status:
- During active flare-ups: Strict low-fiber diet (less than 15g daily) for short-term healing
- Recovery phase: Gradual fiber increase (2-3g daily) over 2-4 weeks
- Maintenance phase: Target 25-30g fiber daily from diverse sources
- Preventive approach: High-fiber diet shown to reduce recurrence risk by 30-40% according to Mayo Clinic research
Important context boundaries: These recommendations apply specifically to diverticulitis (inflamed diverticula), not diverticulosis (pouches without inflammation). If you've had complications like abscesses or perforations, your gastroenterologist may provide more stringent guidelines.
Evidence-Based Food Choices
Rather than focusing solely on restrictions, build your diet around these research-supported options:
- Soluble fiber sources: Oatmeal, peeled apples, and cooked carrots help form protective gel in the colon
- Lean proteins: Fish, poultry, and eggs support healing without digestive strain
- Probiotic-rich foods: Yogurt with live cultures may support gut microbiome balance
- Healthy fats: Olive oil and avocado provide anti-inflammatory benefits
The American College of Gastroenterology notes that a Mediterranean-style diet—rich in vegetables, fruits, whole grains, and healthy fats—shows particular promise for reducing diverticulitis recurrence. Remember that individual tolerance varies significantly, so work with your healthcare provider to develop a personalized plan.
Debunking Common Misconceptions
Several persistent myths about diverticulitis diet lack scientific support:
- "Seeds and nuts get stuck in diverticula": Multiple studies, including research in Clinical Gastroenterology and Hepatology, found no association between seed/nut consumption and diverticulitis complications
- "You must avoid all high-fiber foods forever": Long-term high-fiber diets actually reduce recurrence risk by promoting regular bowel movements
- "Diverticulitis only affects older adults": Incidence is rising among younger populations, often linked to dietary patterns
When evaluating dietary advice, always check if recommendations are supported by current medical literature rather than anecdotal experiences. The shift from restrictive to personalized approaches reflects medicine's growing understanding of individual variation in digestive health.
Implementing Your Dietary Plan
Transitioning to a diverticulitis-friendly diet requires careful planning:
- Consult your gastroenterologist before making significant dietary changes
- During flare-ups, follow medical advice for liquid or low-residue diets
- Gradually increase fiber by 2-3 grams daily to avoid gas and bloating
- Track food intake and symptoms in a journal for 4-6 weeks
- Reintroduce potentially problematic foods one at a time
- Schedule regular follow-ups with your healthcare provider
Remember that proper hydration is equally important—aim for 8-10 glasses of water daily when increasing fiber intake. The Academy of Nutrition and Dietetics emphasizes that sudden, drastic dietary changes often lead to poor adherence and suboptimal results.
Frequently Asked Questions
Can I eat nuts and seeds with diverticulitis?
Yes, current research shows most people with diverticulitis can safely consume nuts and seeds. Earlier recommendations to avoid them were based on theoretical concerns without scientific evidence. However, during acute flare-ups, your doctor may temporarily recommend avoiding them until inflammation subsides.
What is the best diet for preventing diverticulitis flare-ups?
A high-fiber diet (25-30g daily) with adequate hydration is recommended for prevention. Focus on soluble fiber sources like oats, cooked vegetables, and peeled fruits. The Mediterranean diet pattern shows particular effectiveness. Always implement dietary changes gradually and under medical supervision.
How long should I follow a low-fiber diet during a flare-up?
Typically 2-4 days during acute symptoms, followed by a gradual transition to higher fiber over 2-4 weeks. The exact duration depends on symptom severity and your doctor's assessment. Never maintain a low-fiber diet longer than medically necessary, as this may increase recurrence risk.
Are there specific fruits I should avoid with diverticulitis?
During flare-ups, avoid raw fruits with skins and seeds (berries, figs). In remission, most fruits are acceptable when properly prepared—peeled apples, ripe bananas, and cooked pears are generally well-tolerated. Introduce new fruits gradually to assess individual tolerance.
Does alcohol affect diverticulitis?
Excessive alcohol consumption may increase diverticulitis risk and complications. During flare-ups, avoid alcohol completely as it can irritate the digestive tract. In remission, moderate consumption (1 drink/day for women, 2 for men) is generally acceptable for most people, but discuss with your doctor.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4