If you have a stomach ulcer, avoid spicy foods, citrus fruits, coffee, alcohol, and high-fat foods as they can worsen symptoms. Modern research shows diet alone doesn't cause ulcers (most are from H. pylori bacteria or NSAIDs), but certain foods can aggravate pain and delay healing. This guide provides evidence-based dietary recommendations to manage ulcer symptoms while supporting medical treatment.
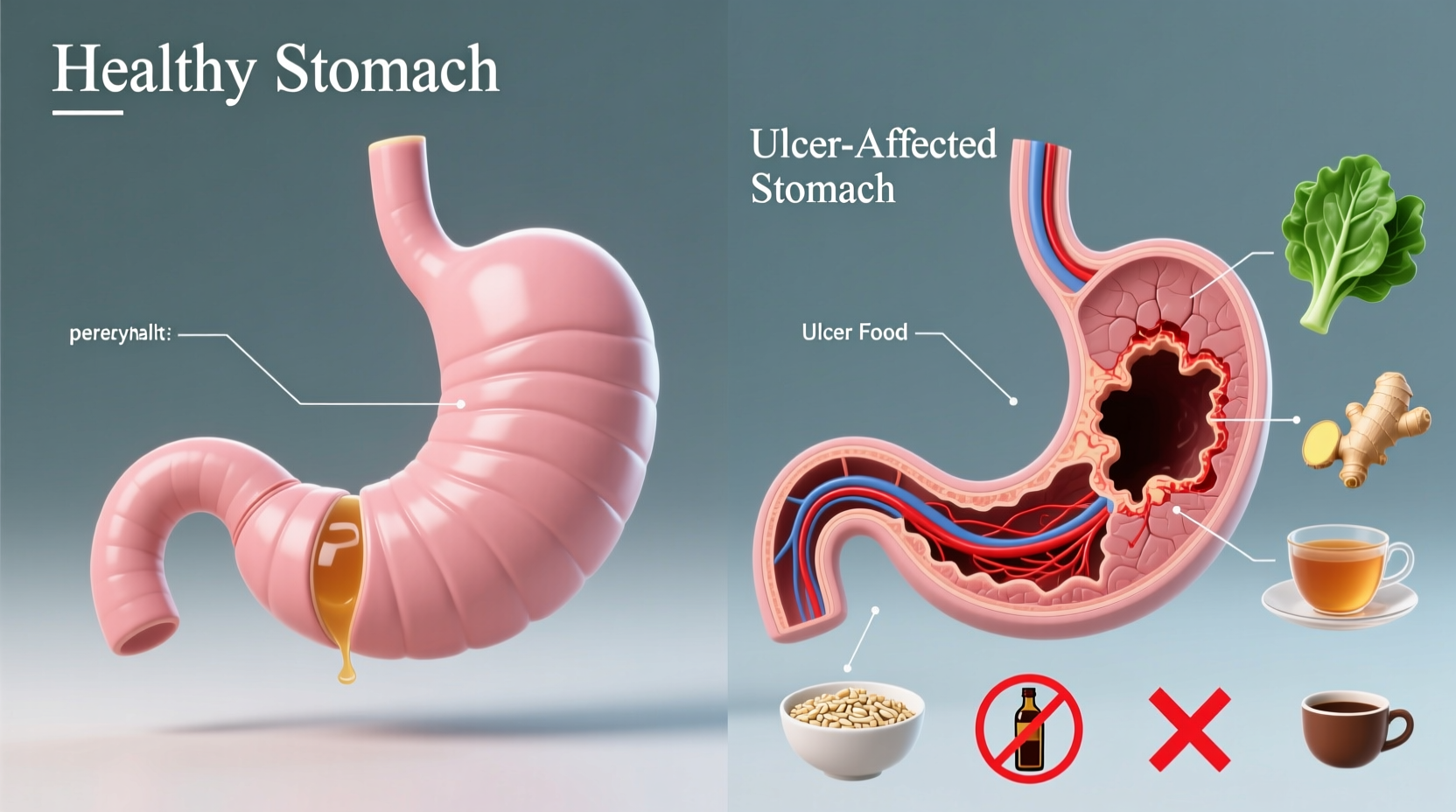
When managing a stomach ulcer, understanding which foods to avoid is crucial for symptom relief and healing. Contrary to popular belief, ulcers aren't primarily caused by diet—most result from Helicobacter pylori bacterial infection or prolonged NSAID use. However, specific foods can irritate the stomach lining, increase acid production, and worsen discomfort. This comprehensive guide outlines exactly which foods to avoid with an ulcer, explains why they're problematic, and provides practical alternatives backed by current medical research from gastroenterology experts.
Understanding Ulcer Triggers: Beyond the Myths
For decades, ulcer patients were prescribed highly restrictive "bland diets" with little scientific basis. Modern research from the National Institute of Diabetes and Digestive and Kidney Diseases reveals that while diet doesn't cause ulcers, certain foods can significantly aggravate symptoms during active healing. The key is identifying your personal triggers while supporting medical treatment.
Foods That Directly Irritate Ulcer Sites
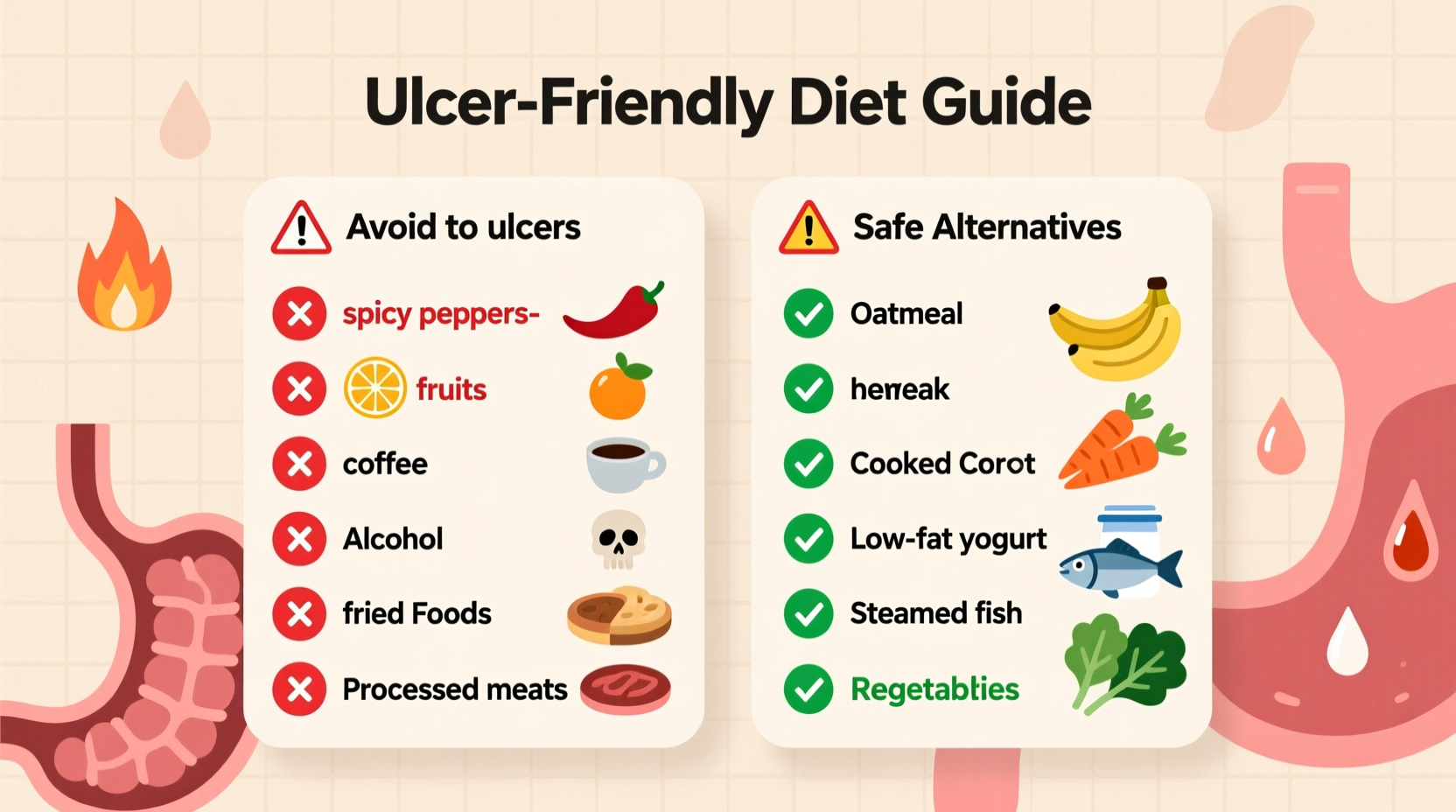
These foods consistently cause problems for ulcer patients by increasing stomach acid or directly irritating the stomach lining:
| Foods to Avoid | Why They're Problematic | Better Alternatives |
|---|---|---|
| Spicy peppers (chili, cayenne) | Stimulate acid production and irritate ulcer sites | Mild herbs like basil, oregano, turmeric |
| Citrus fruits and juices | High acidity worsens ulcer pain | Melons, bananas, apples |
| Coffee (including decaf) | Increases gastric acid secretion by 70-90% | Chamomile tea, water, almond milk |
| Alcohol (all types) | Irritates stomach lining and increases acid | Non-alcoholic beverages |
| Carbonated beverages | Gas bubbles expand stomach, increasing pressure on ulcers | Still water, herbal infusions |
Individual Trigger Foods: The Gray Area
Unlike the universally problematic foods above, these items affect people differently. Keep a food diary to identify your personal triggers:
- Fatty foods: Fried items and high-fat meats can delay stomach emptying, increasing acid exposure time
- Tomato products: While acidic like citrus, some ulcer patients tolerate small amounts
- Chocolate: Contains methylxanthines that may relax the lower esophageal sphincter
- Peppermint: Often thought to soothe digestion but can worsen ulcer symptoms for some
According to a Mayo Clinic analysis of patient reports, approximately 68% of ulcer sufferers identify specific food triggers beyond the universally problematic categories. This highlights why personalized dietary adjustments are essential.
Timing Matters: When to Restrict Certain Foods
Even generally safe foods can cause issues depending on timing. Understanding this ulcer management timeline helps optimize your diet:
| Healing Phase | Dietary Focus | Foods to Temporarily Limit |
|---|---|---|
| Acute phase (first 1-2 weeks) | Maximum protection | All spicy foods, citrus, coffee, alcohol, fatty foods |
| Early healing (2-6 weeks) | Gradual reintroduction | Mild spices, small citrus portions, lean proteins |
| Maintenance phase (after 6 weeks) | Personalized balance | Most foods with attention to individual tolerance |
This phased approach aligns with current gastroenterology recommendations from the American College of Gastroenterology, which emphasizes that dietary restrictions should become less stringent as ulcers heal, provided medical treatment is effective.
Building an Ulcer-Friendly Meal Plan
Creating meals that support healing requires strategic planning. Follow these practical guidelines:
- Eat smaller, more frequent meals (5-6 daily) to prevent stomach overfilling and reduce acid production spikes
- Cook with gentle methods like steaming, poaching, or baking instead of frying
- Include healing-promoting foods such as probiotic-rich yogurt, honey (in moderation), and cruciferous vegetables
- Wait 2-3 hours after eating before lying down to prevent acid reflux
- Chew thoroughly to reduce digestive workload on your healing stomach
When to Consult Your Healthcare Provider
Dietary changes support but don't replace medical treatment for ulcers. Contact your doctor immediately if you experience:
- Severe or persistent abdominal pain
- Vomiting blood or material that looks like coffee grounds
- Black, tarry stools
- Unintended weight loss
- Symptoms that don't improve with standard treatment
Remember that effective ulcer treatment requires addressing the underlying cause—whether H. pylori infection requiring antibiotics or NSAID-induced damage requiring medication adjustment. Dietary modifications work best when combined with appropriate medical care.
FAQs About Ulcer Diets
Can I ever eat spicy food again with an ulcer?
During active ulcer healing, avoid spicy foods completely. After successful treatment (confirmed by your doctor), many people can gradually reintroduce mild spices. Start with small amounts of herbs like turmeric or oregano before trying hotter spices, and monitor your body's response carefully.
Is milk good for ulcers as previously believed?
While milk may temporarily soothe ulcer pain, it actually stimulates additional acid production within 30-60 minutes. The American College of Gastroenterology no longer recommends milk as an ulcer treatment. Instead, try almond milk or small portions of probiotic yogurt which support healing without triggering excess acid.
How long should I follow an ulcer diet?
Continue strict dietary modifications during active treatment (typically 4-8 weeks). After your doctor confirms healing, gradually reintroduce previously avoided foods while monitoring symptoms. Most people can return to a normal diet within 3-6 months, though some may need to permanently avoid specific personal triggers.
Do all ulcers require the same dietary restrictions?
No—dietary needs vary based on ulcer cause and location. H. pylori-related ulcers often tolerate more foods than NSAID-induced ulcers. Duodenal ulcers (in the small intestine) may have different triggers than gastric ulcers (in the stomach). Your healthcare provider can help tailor dietary recommendations to your specific condition.
Can stress affect ulcer symptoms regardless of diet?
Yes—stress significantly impacts ulcer symptoms by increasing stomach acid production and reducing mucosal protection. Even with perfect dietary management, unmanaged stress can worsen ulcer pain. Incorporate stress-reduction techniques like deep breathing, meditation, or gentle exercise alongside dietary modifications for best results.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4