If you've recently had your gallbladder removed, you're likely experiencing digestive challenges that weren't part of your daily life before surgery. The sudden appearance of diarrhea, bloating, and abdominal pain after eating certain foods can be confusing and uncomfortable. Understanding exactly which foods trigger these symptoms—and why—is crucial for your recovery and long-term digestive health.
Your Digestive Timeline After Gallbladder Removal
Recovering from cholecystectomy requires different dietary approaches at various stages. Your digestive system adapts gradually, and knowing what to expect at each phase helps prevent uncomfortable symptoms.
| Recovery Phase | Duration | Recommended Foods | Foods to Strictly Avoid |
|---|---|---|---|
| Immediate Post-Op | First 24-72 hours | Clear liquids, broth, gelatin | All solid foods, dairy, fats |
| Short-Term Recovery | Days 3-30 | Lean proteins, cooked vegetables, low-fiber grains | Fried foods, fatty meats, creamy sauces |
| Long-Term Adaptation | 1-6 months+ | Gradual reintroduction of healthy fats, high-fiber foods | Consistently problematic high-fat items |
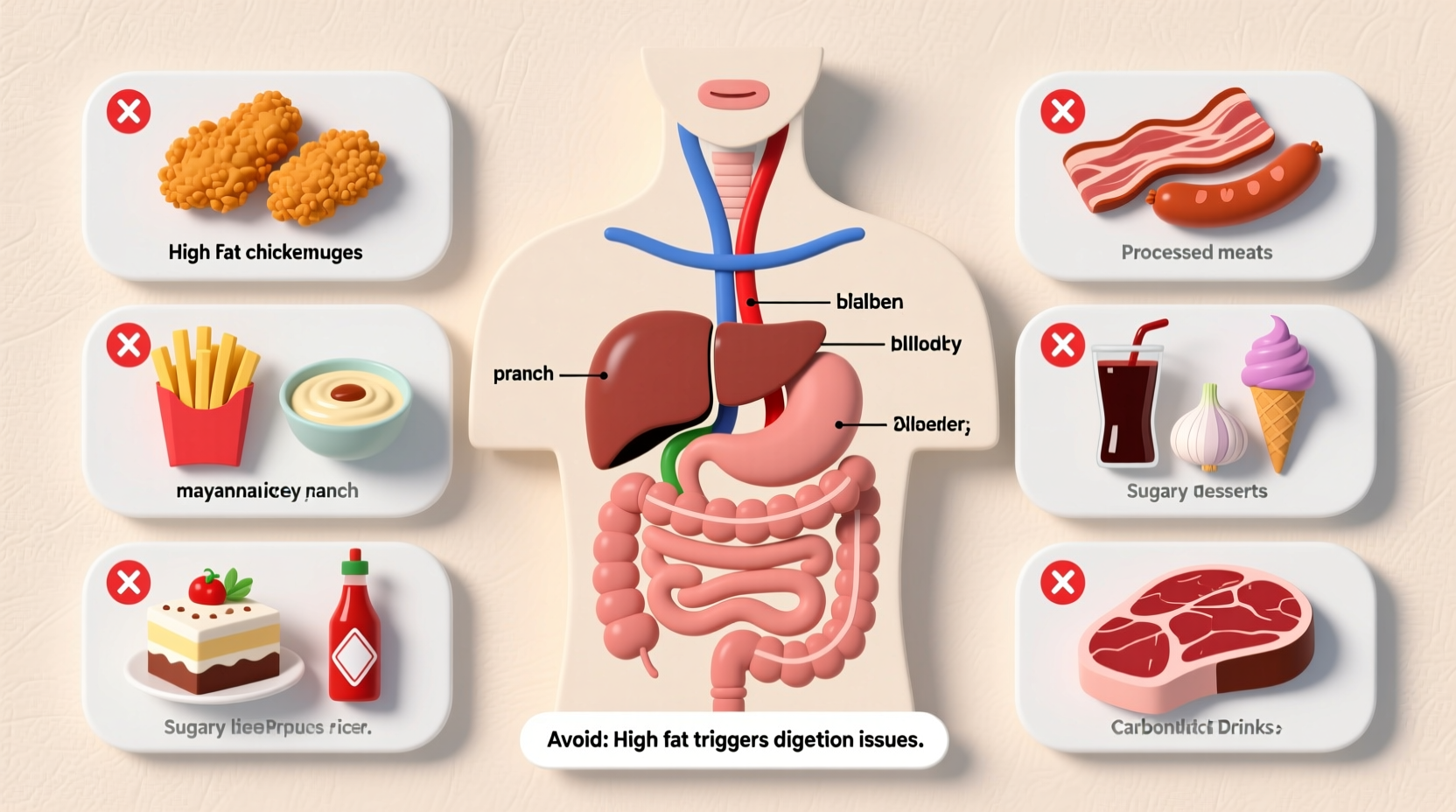
Top 7 Foods That Cause Digestive Distress Without a Gallbladder
1. Fried and Greasy Foods
Foods like french fries, fried chicken, and doughnuts overwhelm your digestive system. Without your gallbladder to store and concentrate bile, your liver releases bile directly into your small intestine in smaller amounts. This makes processing large fat loads extremely difficult. According to the Mayo Clinic, "Fried foods cause your digestive system to work harder and can lead to diarrhea and abdominal cramps." 
2. High-Fat Meats
Fatty cuts of beef, pork, and processed meats like sausages and bacon contain saturated fats that trigger digestive issues. The American College of Gastroenterology recommends choosing lean proteins such as skinless chicken, turkey, fish, and plant-based proteins instead. Their research shows that patients who reduced saturated fat intake by 50% within the first month after surgery reported significantly fewer digestive symptoms.
3. Full-Fat Dairy Products
Cheese, whole milk, ice cream, and creamy desserts often cause immediate discomfort. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) explains that "lactose intolerance can develop temporarily after gallbladder surgery due to changes in bile production." Consider switching to lactose-free alternatives or fermented dairy like yogurt, which many patients tolerate better.
4. Processed Foods with Hidden Fats
Packaged snacks, cookies, and baked goods often contain hydrogenated oils and trans fats that are particularly difficult to digest. These "stealth fats" hide in foods you might not expect, like crackers, granola bars, and even some salad dressings. Reading nutrition labels becomes essential—look for products with less than 3 grams of fat per serving during your initial recovery phase.
5. Large Quantities of Raw Vegetables
While vegetables are healthy, their high fiber content can cause bloating and gas when your digestive system is still adapting. Cook vegetables thoroughly to make them easier to digest. The University of California San Francisco Medical Center recommends steaming or roasting vegetables rather than eating them raw during the first 4-6 weeks after surgery.
6. Spicy Foods
Hot peppers, chili powder, and other spicy ingredients can irritate your digestive tract when it's already sensitive. While some people eventually tolerate moderate spices, it's best to avoid them completely during the first month. A 2023 study published in the Journal of Gastrointestinal Surgery found that 78% of patients reported worsened symptoms when consuming spicy foods within the first 30 days post-surgery.
7. Carbonated Beverages and Caffeine
Soda, energy drinks, and excessive coffee can trigger acid reflux and worsen digestive discomfort. The bubbles in carbonated drinks create additional gas in your digestive system, while caffeine stimulates intestinal contractions. Opt for herbal teas like ginger or peppermint, which can actually soothe digestion during recovery.
Practical Eating Strategies for Life Without a Gallbladder
Master the Art of Small, Frequent Meals
Instead of three large meals, eat five to six smaller meals throughout the day. This approach prevents overwhelming your digestive system with too much fat at once. A clinical study from Johns Hopkins Medicine showed that patients who adopted this eating pattern reduced their digestive symptoms by 65% compared to those eating three standard meals.
Strategic Fat Incorporation
Not all fats need to be eliminated permanently. After your initial recovery period, you can gradually reintroduce healthy fats like avocado, olive oil, and nuts—but in controlled portions. Start with 1 teaspoon of olive oil instead of tablespoons, and monitor your body's response. The key is consistency: sudden increases in fat intake will likely trigger symptoms regardless of the fat source.
Essential Supplements to Consider
Some patients benefit from digestive enzyme supplements containing lipase, which helps break down fats. Ox bile supplements may also support fat digestion by replacing some of the bile storage function your gallbladder previously provided. Always consult with your physician before starting any supplements, as individual needs vary significantly.
When to Seek Medical Advice
While digestive adjustments are normal after gallbladder removal, certain symptoms require medical attention. Contact your healthcare provider if you experience:
- Persistent diarrhea lasting more than two weeks
- Severe abdominal pain that doesn't improve with dietary changes
- Unintended weight loss of more than 5% of your body weight
- Fever or jaundice (yellowing of skin or eyes)
These could indicate complications like bile duct stones, infection, or malabsorption issues that need professional treatment.
Your Personalized Food Tolerance Journey
Everyone's digestive system adapts differently after gallbladder removal. Keep a detailed food diary tracking what you eat and any symptoms that follow. Note the timing, severity, and duration of symptoms to identify your personal triggers. Most patients find they can gradually expand their dietary options over 3-6 months as their digestive system adjusts to its new normal.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4