When diverticulitis strikes, knowing exactly what to eat—and what to avoid—can mean the difference between a quick recovery and prolonged discomfort. This evidence-based guide cuts through outdated myths and delivers current medical recommendations you can trust.
Understanding Diverticulitis and Dietary Impact
Diverticulitis occurs when small pouches in your colon wall (diverticula) become inflamed or infected. During acute flare-ups, your digestive system needs rest. What you eat directly impacts healing time and symptom severity. The American Gastroenterological Association emphasizes that dietary choices during flare-ups significantly influence recovery outcomes.
Immediate Dietary Restrictions During Flare-Ups
When symptoms hit—abdominal pain, fever, nausea—you need to modify your diet immediately. During acute episodes, healthcare providers typically recommend:
- Clear liquid diet for initial 24-48 hours (broth, apple juice, gelatin)
- Progression to low-fiber diet as symptoms improve (white rice, eggs, cooked carrots)
- Complete avoidance of high-fiber foods until inflammation subsides
| Foods to Avoid During Flare-Ups | Why They're Problematic | Safe Alternatives |
|---|---|---|
| Whole grains (brown rice, quinoa) | Too much fiber increases colon movement | White rice, refined pasta |
| Raw vegetables and fruits | Difficult to digest during inflammation | Cooked carrots, applesauce |
| Nuts and seeds | Historically thought to lodge in diverticula | Smooth nut butters (in recovery phase) |
| Popcorn | Hard hulls potentially irritating | Rice cakes (well-chewed) |
| Beans and legumes | High fiber causes gas and bloating | Canned lentils (well-cooked) |
Evolving Medical Recommendations: What's Changed
Medical understanding of diverticulitis dietary management has evolved significantly. The timeline below shows how recommendations have shifted based on new evidence:
- 1950s-2000s: Strict avoidance of nuts, seeds, and popcorn universally recommended
- 2011: Harvard study tracking 47,000 men found no increased risk from nuts or popcorn
- 2018: American Gastroenterological Association updates guidelines reflecting new evidence
- Present: Individualized approach based on patient history and severity
"Current evidence doesn't support the routine restriction of nuts, seeds, and popcorn for preventing diverticulitis complications," states Dr. Anne Peery, lead author of the 2018 American Gastroenterological Association guidelines. This represents a significant shift from previous decades of dietary advice.
Context-Specific Dietary Guidance
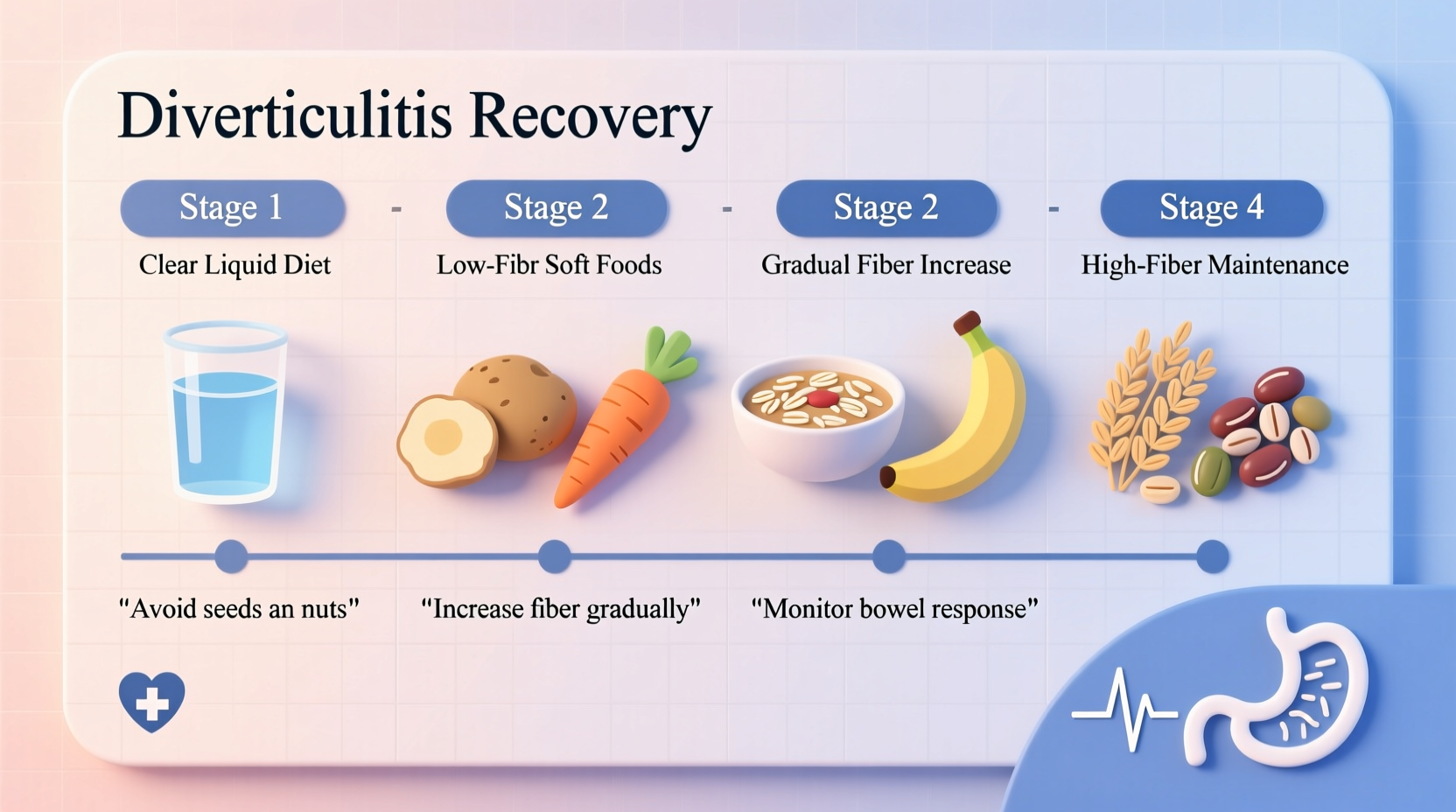
Your dietary needs vary significantly depending on your current condition phase:
- Acute flare-up: Strict low-fiber diet (less than 10g fiber daily)
- Recovery phase: Gradual fiber increase over 2-4 weeks
- Long-term maintenance: High-fiber diet (25-30g daily) to prevent recurrence
The Mayo Clinic emphasizes that dietary restrictions should be temporary during active inflammation. Long-term, a high-fiber diet actually reduces recurrence risk by 31% according to research published in the Journal of Gastroenterology.
Practical Meal Planning Strategies
Navigating diverticulitis-friendly eating doesn't mean bland meals. Try these practical approaches:
- Flare-up friendly breakfast: White toast with smooth almond butter, scrambled eggs
- Recovery phase lunch: Bland chicken soup with well-cooked noodles, canned peaches
- Maintenance dinner: Baked salmon with roasted zucchini and quinoa
When reintroducing fiber, increase gradually by 5g per day. Sudden increases can trigger symptoms. Keep a food diary to identify personal triggers—individual responses vary significantly.
When to Consult Your Healthcare Provider
Dietary management should complement—not replace—medical treatment. Contact your healthcare provider if:
- Fever exceeds 100.4°F (38°C)
- Pain worsens despite dietary changes
- Symptoms persist beyond 48 hours on clear liquids
- You experience vomiting or inability to keep liquids down
Nutrition counseling with a registered dietitian specializing in gastrointestinal conditions provides personalized guidance based on your specific health profile and dietary history.











 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4