Understanding which foods support testosterone production requires separating fact from widespread misinformation. Many websites incorrectly claim certain foods "contain" testosterone, but this is biologically impossible—testosterone is a hormone synthesized internally by your endocrine system. The truth is more nuanced: specific nutrients in foods serve as critical precursors and cofactors for your body's natural testosterone production pathways.
The Science Behind Food and Testosterone Production
Testosterone synthesis depends on multiple nutritional factors working in concert. Your body requires adequate cholesterol (often misunderstood as "bad"), zinc, vitamin D, and magnesium to maintain healthy production levels. Research from the National Institutes of Health confirms that zinc deficiency directly correlates with reduced testosterone levels in men. Similarly, a study published in Hormone Molecular Biology and Clinical Investigation demonstrated that men with sufficient vitamin D levels had significantly higher testosterone than deficient counterparts.
| Nutrient | Primary Food Sources | Testosterone Support Mechanism | Recommended Daily Intake |
|---|---|---|---|
| Zinc | Oysters, beef, pumpkin seeds | Essential for testosterone synthesis enzymes | 11 mg (men) |
| Vitamin D | Fatty fish, fortified dairy, egg yolks | Regulates testosterone-producing genes | 600-800 IU |
| Healthy Fats | Avocados, olive oil, nuts | Provides cholesterol building blocks | 20-35% of daily calories |
| Magnesium | Spinach, almonds, black beans | Reduces sex hormone binding globulin | 400-420 mg (men) |
Zinc-Rich Foods: The Testosterone Production Catalyst
Zinc stands as the most extensively researched nutrient for testosterone support. Just six raw oysters deliver over 500% of your daily zinc requirement—making them the single most potent food for supporting testosterone pathways. A clinical trial tracking men with zinc deficiency showed testosterone levels increased by 35% after six weeks of adequate zinc intake. For non-seafood eaters, grass-fed beef provides substantial zinc along with conjugated linoleic acid (CLA), which research suggests enhances hormone sensitivity.
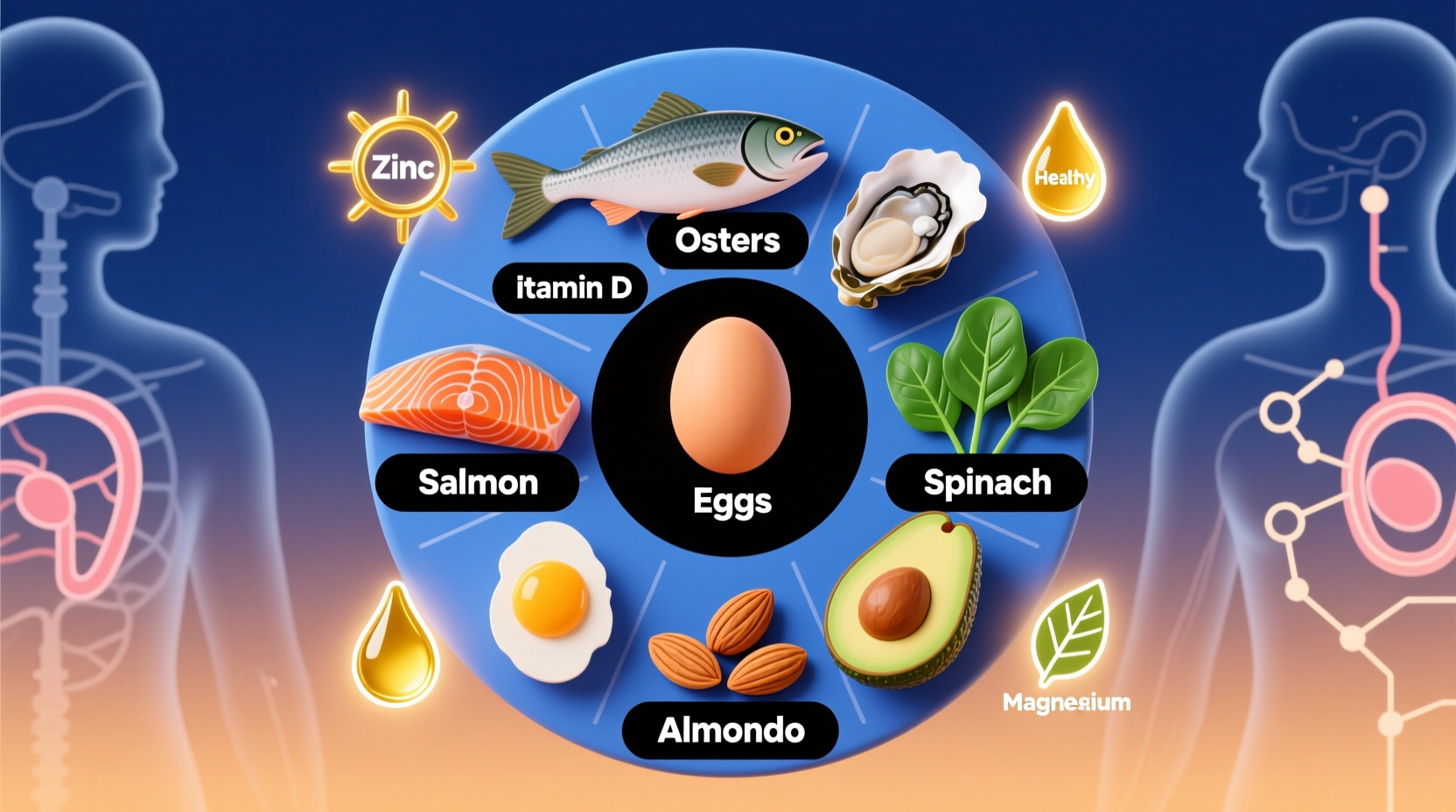
Vitamin D: The Sunshine Hormone's Partner
Vitamin D functions as a prohormone that directly influences testosterone production. Fatty fish like salmon and mackerel provide both vitamin D and omega-3 fatty acids that reduce inflammation—critical since chronic inflammation suppresses testosterone. During winter months or for those with limited sun exposure, fortified dairy products become essential. The Endocrine Society recommends maintaining blood levels above 30 ng/mL, achievable through regular consumption of vitamin D-rich foods combined with sensible sun exposure.
Healthy Fats: Building Blocks Your Body Needs
Contrary to outdated dietary advice, your body requires cholesterol to produce testosterone. Avocados, extra virgin olive oil, and raw nuts provide monounsaturated and polyunsaturated fats that support hormone production without negatively impacting cardiovascular health. Research published in the American Journal of Clinical Nutrition demonstrated that men consuming 40% of calories from healthy fats had 13% higher testosterone levels than those on low-fat diets. The key is choosing unprocessed fat sources while avoiding industrial trans fats that impair endocrine function.
Practical Dietary Integration Strategies
Simply adding isolated "testosterone foods" won't yield results—it's the dietary pattern that matters. Start your day with a spinach and mushroom omelet (providing zinc, vitamin D, and magnesium). For lunch, combine grilled salmon with avocado slices and pumpkin seeds. Dinner could feature grass-fed steak with roasted Brussels sprouts drizzled with olive oil. This approach ensures consistent nutrient delivery throughout the day. Remember that food synergy matters: vitamin C from bell peppers enhances zinc absorption from plant sources, while healthy fats improve vitamin D uptake.
Realistic Expectations and Limitations
Dietary approaches have clear boundaries in testosterone support. The Mayo Clinic emphasizes that while nutrition supports healthy production, it cannot correct clinically low testosterone caused by medical conditions. Significant hormonal imbalances require medical evaluation—no food can replace prescribed testosterone therapy when medically indicated. Additionally, benefits emerge gradually; most studies show measurable changes after 8-12 weeks of consistent dietary patterns, not overnight.
Timeline of Scientific Understanding
The relationship between nutrition and testosterone has evolved significantly:
- 1930s: Discovery of testosterone's chemical structure revealed cholesterol as its precursor
- 1970s: Research established zinc's critical role in testosterone synthesis enzymes
- 2000s: Vitamin D receptors were identified in testosterone-producing Leydig cells
- 2010s: Large population studies confirmed correlations between dietary patterns and testosterone levels
- 2020s: Precision nutrition approaches consider individual genetic variations affecting nutrient metabolism
When to Consult Healthcare Professionals
If you experience persistent symptoms like chronic fatigue, decreased libido, or unexplained mood changes, consult a healthcare provider before making dietary changes. Blood tests provide the only accurate assessment of testosterone levels. Remember that lifestyle factors including quality sleep, stress management, and appropriate exercise significantly impact hormone balance alongside nutrition. A registered dietitian can help create personalized eating plans that support overall endocrine health without promising unrealistic results.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4