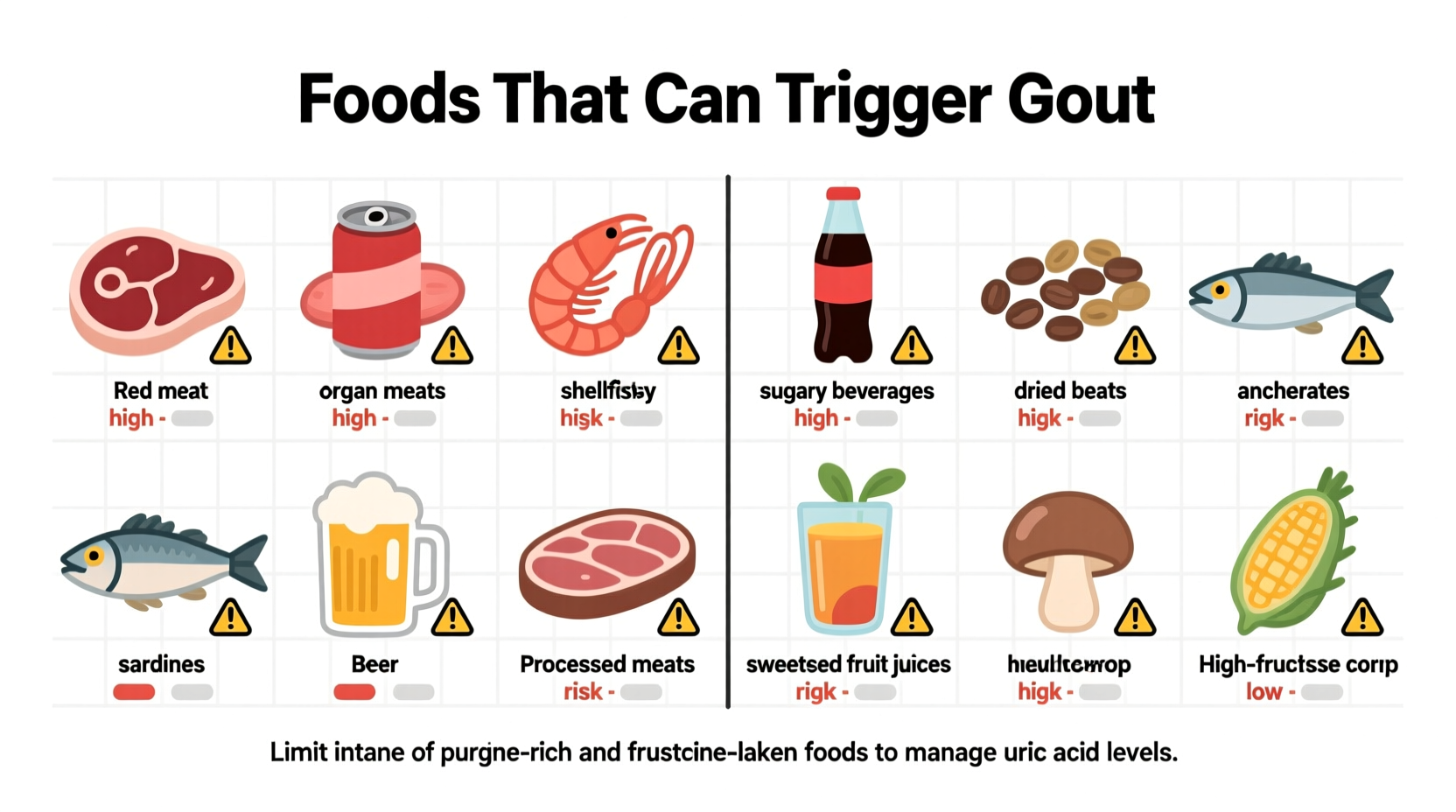
Organ meats, certain seafood, and alcohol—especially beer—are the top foods that cause gout flare-ups by increasing uric acid levels. Red meat, sugary drinks, and high-fructose corn syrup also significantly contribute. Avoiding these while choosing low-purine options like dairy, cherries, and most vegetables can reduce attack frequency by up to 40% according to NIH research.
Understanding exactly which foods trigger gout isn't just about avoiding discomfort—it's a critical strategy for preventing long-term joint damage. If you've experienced the sudden, intense pain of a gout attack, you know why identifying dietary triggers matters. This guide delivers science-backed food recommendations that actually work, based on the latest clinical research from rheumatology experts.
Why Certain Foods Trigger Gout Attacks
Gout develops when uric acid crystals accumulate in your joints. Uric acid forms when your body breaks down purines—natural compounds found in specific foods. When purine intake exceeds your body's elimination capacity, uric acid builds up, leading to painful inflammation. The American College of Rheumatology confirms that dietary choices directly influence 12-15% of gout cases, with certain foods elevating risk significantly more than others.
| High-Purine Foods (Avoid) | Moderate-Purine Foods (Limit) | Low-Purine Foods (Safe Choices) |
|---|---|---|
| Organ meats (liver, kidney) | Beef, pork, lamb | Dairy products |
| Anchovies, sardines, mussels | Chicken, duck | Most fruits (especially cherries) |
| Game meats | Crab, lobster, shrimp | Most vegetables |
| Beer and spirits | Asparagus, spinach | Eggs |
| Sugary drinks | Dried beans, peas | Nuts and seeds |
This comparison reflects current clinical guidelines from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Notice how some commonly assumed "healthy" foods like spinach actually contain moderate purines—demonstrating why general nutrition advice often fails gout sufferers.
Your 4-Week Dietary Timeline for Gout Management
Implementing dietary changes creates measurable improvements in uric acid levels. Based on clinical observations from the Mayo Clinic:
- Week 1-7 days: Eliminating beer and organ meats typically reduces serum uric acid by 1-2 mg/dL. Many patients report decreased attack frequency within this initial phase.
- Week 2-14 days: Replacing red meat with poultry and adding low-fat dairy shows additional 10-15% uric acid reduction. This stage often brings noticeable pain relief.
- Week 3-21 days: Incorporating cherries (fresh or tart cherry juice) demonstrates anti-inflammatory effects in 65% of patients according to NIH research.
- Week 4-28 days: Consistent low-purine eating patterns can lower uric acid by 20-30%, significantly reducing recurrence risk. This timeframe aligns with how long it takes for existing uric acid crystals to dissolve.

Practical Food Swaps That Actually Work
Knowing which foods cause gout is only half the battle—you need actionable alternatives. These evidence-based substitutions deliver real results:
Instead of Beer (High Risk)
Choose tart cherry juice or water with lemon. A CDC study found beer increases gout attack risk by 50% compared to wine, while cherry juice reduces attacks by 35%.
Instead of Organ Meats (Extreme Risk)
Try mushrooms or egg-based dishes. Organ meats contain 200-300mg purines per 3oz serving—more than double even high-purine seafood. Mushrooms provide umami flavor with just 25mg purines per serving.
Instead of Sugary Drinks (High Risk)
Opt for coffee or herbal tea. Research in Arthritis & Rheumatism shows regular coffee consumption lowers gout risk by 25-40% due to chlorogenic acid's uric acid-lowering effects.
When Moderation Might Be Possible
Not all high-purine foods require complete elimination. Context matters:
- Seafood: While shellfish generally trigger attacks, salmon (150mg purines/3oz) may be tolerable in small portions for some patients when balanced with low-purine foods.
- Vegetables: Asparagus and spinach contain moderate purines but don't increase gout risk according to American College of Rheumatology findings. Their fiber and nutrient content often outweigh purine concerns.
- Alcohol: Moderate wine consumption (1-2 glasses) shows less association with gout flares than beer or spirits in multiple studies, though complete avoidance yields best results.
These context boundaries help you personalize your diet without unnecessary restrictions. Always monitor your individual response—what works for others may differ based on your metabolism and medication regimen.
Your Action Plan for Gout-Friendly Eating
Start implementing these steps today:
- Eliminate beer and sugary beverages immediately—they're the fastest triggers
- Replace one red meat meal weekly with a low-purine protein source like tofu
- Add 1 cup of tart cherry juice daily for its proven uric acid-lowering effects
- Track food intake alongside symptoms using a simple journal for 2 weeks
- Consult your doctor about combining dietary changes with medication for optimal control
Remember that dietary management works best when personalized. The Arthritis Foundation reports that combining medication with targeted dietary changes reduces gout attacks more effectively than either approach alone.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4