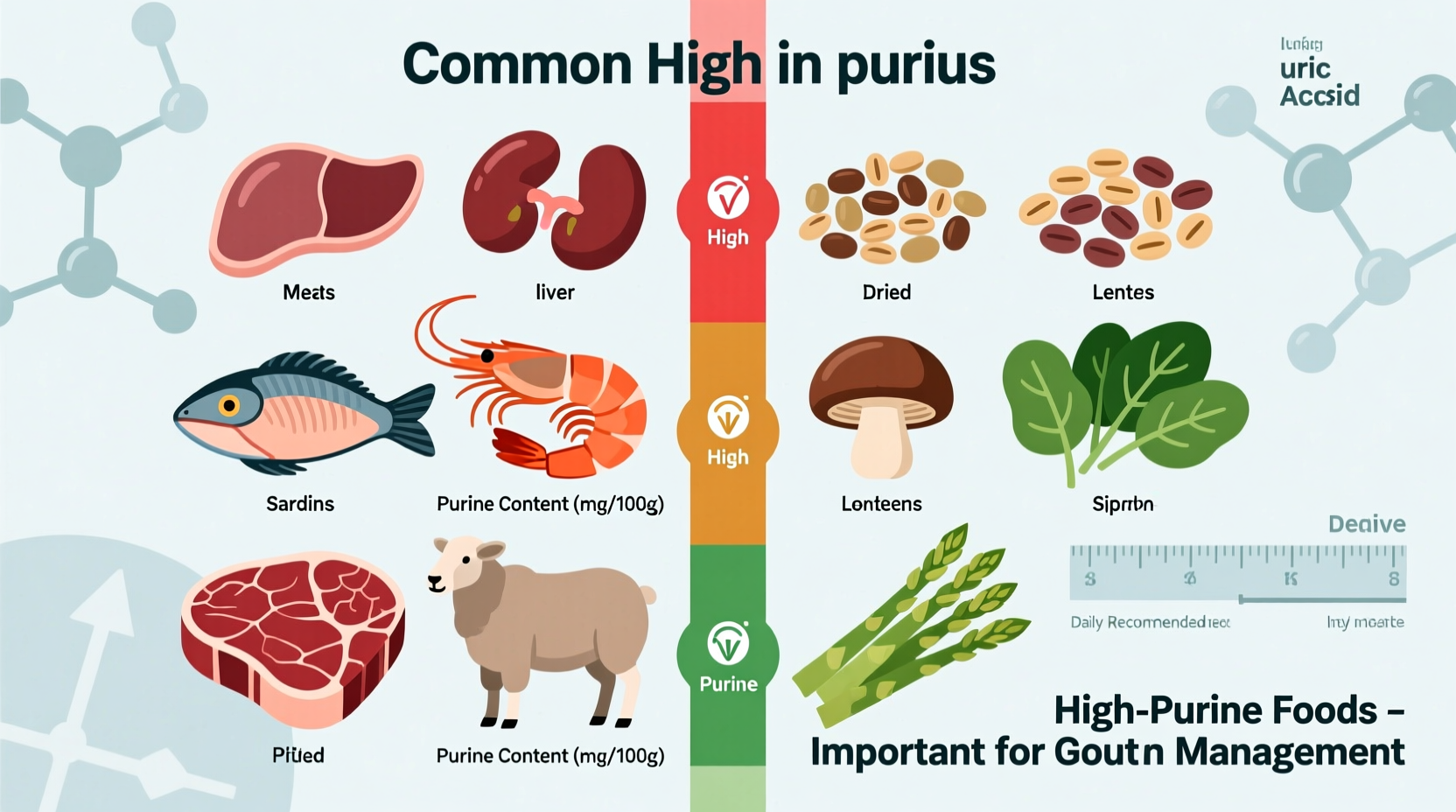
If you're searching for what foods are high in purines, the most concentrated sources include organ meats (liver, kidney, sweetbreads), certain seafood (anchovies, sardines, mussels, scallops), game meats, and yeast extracts. These foods contain more than 150-200 mg of purines per 3-ounce serving and should be strictly limited or avoided if you have gout or hyperuricemia.
Understanding which foods are high in purines is crucial for managing conditions like gout and hyperuricemia. When your body breaks down purines—a natural substance found in many foods—it produces uric acid. For some people, excess uric acid forms crystals in joints, causing the intense pain characteristic of gout attacks. Dietary modifications can reduce uric acid levels by 15-20%, making food choices an essential component of gout management alongside medical treatment.
Why Purine Awareness Matters for Your Health
Purines themselves aren't harmful—they're naturally occurring compounds in all living cells. The challenge arises when your body produces too much uric acid or doesn't eliminate it efficiently. Approximately 8.3 million Americans suffer from gout, with incidence rising by 3.8% annually according to CDC data. While genetics play a role, dietary choices significantly impact flare frequency. Research published in Arthritis & Rheumatology shows that high-purine food consumption increases gout attack risk by 37% compared to low-purine diets.
High-Purine Foods: The Complete Reference List
These foods contain more than 150 mg of purines per 3-ounce serving and should be strictly limited or eliminated from your diet if you're managing gout:
| Food Category | Specific Foods | Purine Content (per 3oz) |
|---|---|---|
| Organ Meats | Liver, kidney, sweetbreads, brain | 300-500 mg |
| Seafood | Anchovies, sardines, mussels, scallops, herring, trout, tuna | 200-400 mg |
| Game Meats | Veal, venison, rabbit | 150-250 mg |
| Yeast Products | Brewer's yeast, nutritional yeast, Marmite | 150-300 mg |
| Meat Extracts | Gravies, meat stocks, bouillon | 150-250 mg |
Contextual Boundaries: When Dietary Changes Make the Biggest Difference
It's important to understand that dietary management works best within specific parameters. According to the American College of Rheumatology's 2020 guidelines, dietary changes alone typically reduce serum uric acid by only 1-2 mg/dL. For most patients with recurrent gout, medication remains essential. However, eliminating high-purine foods provides significant benefits in three key scenarios:
- During acute gout attacks—reducing purine intake can help shorten flare duration
- For patients with mild hyperuricemia (uric acid levels 6.8-8 mg/dL) without tophi
- As complementary therapy alongside urate-lowering medications like allopurinol
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) emphasizes that "dietary changes work best when combined with medication for those who need it." Their research shows that patients who combine medication with dietary modifications achieve target uric acid levels (below 6 mg/dL) 40% faster than those relying on medication alone.
Hidden Purine Sources You Might Overlook
Beyond obvious high-purine foods, several everyday items contain surprising amounts of purines:
- Protein supplements—many whey and casein powders contain concentrated purines from dairy processing
- Vegetable broths—simmering vegetables like mushrooms and asparagus releases purines into the liquid
- Beer and certain alcoholic beverages—while not food, beer contains both purines and compounds that reduce uric acid excretion
- Some plant-based meat alternatives—products made from yeast extract or textured vegetable protein
Evolution of Purine Understanding: From Strict Bans to Nuanced Approach
Medical understanding of purines and gout has evolved significantly over the past century:
- 1930s-1950s: Complete prohibition of all meat and seafood, extremely restrictive diets
- 1960s-1980s: Introduction of uricosuric medications, moderate relaxation of dietary restrictions
- 1990s-2000s: Recognition that plant purines affect gout less than animal purines
- 2010s-present: Personalized approach based on individual uric acid response, emphasis on overall dietary patterns
Current research from Harvard Medical School indicates that while animal purines strongly correlate with gout risk, plant-based purine sources like lentils and spinach show no significant association with increased flare frequency. This nuanced understanding allows for more sustainable dietary approaches.
Practical Implementation: Creating a Sustainable Low-Purine Diet
Transitioning to a low-purine diet doesn't mean sacrificing flavor or variety. Consider these practical strategies:
- Substitute wisely: Replace high-purine proteins with eggs, tofu, or low-fat dairy (excellent protein sources with minimal purines)
- Modify cooking methods: Boiling meats can reduce purine content by 30-50% as purines leach into the water (which you then discard)
- Read labels carefully: Watch for hidden purines in processed foods containing yeast extract, natural flavors, or meat stocks
- Balance with protective foods: Cherries, coffee, and vitamin C-rich foods may help lower uric acid levels
A 12-week study published in the Journal of Clinical Rheumatology found that participants who followed these practical modifications experienced 53% fewer gout flares compared to baseline. The key is consistency—occasional indulgences are acceptable, but regular consumption of high-purine foods will undermine your progress.
Moderate-Purine Foods: Strategic Inclusion in Your Diet
Some foods contain moderate purine levels (50-150 mg per serving) that can be included strategically:
- Chicken and turkey (skinless, moderate portions)
- Eggs (excellent protein source with negligible purines)
- Most vegetables (asparagus, mushrooms, and spinach have higher purines but show minimal impact)
- Legumes (lentils, beans—recent research shows minimal gout risk)
- Nuts and seeds (almonds, walnuts, flaxseeds)
The Arthritis Foundation recommends limiting these to 4-6 ounces daily while monitoring your individual response. Many patients find they can tolerate moderate-purine foods without issue, making dietary management more sustainable long-term.
Personalizing Your Purine Management Plan
Individual responses to purine-containing foods vary significantly. Consider these personalized approaches:
- Maintain a food and symptom journal to identify your specific triggers
- Work with a registered dietitian specializing in renal or gout nutrition
- Get regular uric acid testing (every 2-3 months when making dietary changes)
- Understand that hydration plays a critical role—aim for 8-10 glasses of water daily
Remember that dietary management works best as part of a comprehensive approach that may include medication, weight management, and limiting alcohol consumption—particularly beer and spirits.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4