Current medical evidence shows that seeds, nuts, and popcorn DON'T worsen diverticulosis as previously believed. The primary dietary triggers for diverticulosis complications are low-fiber foods, excessive red meat, and individual-specific irritants that vary by person. A high-fiber diet (25-30g daily) is now recommended to prevent diverticulitis flare-ups, contrary to outdated avoidance advice.
Understanding Diverticulosis and Your Diet
If you've been diagnosed with diverticulosis, you're probably searching for clear answers about which foods might trigger complications. The good news: modern research has overturned decades of dietary myths about this common condition affecting over 50% of Americans over 60. Let's cut through the confusion with evidence-based guidance you can trust.
Diverticulosis vs. Diverticulitis: Why the Distinction Matters
Before discussing problematic foods, it's crucial to understand the difference between these related conditions:
- Diverticulosis: Presence of small pouches (diverticula) in the colon wall, typically asymptomatic
- Diverticulitis: Inflammation or infection of these pouches, causing pain and requiring medical treatment
Your dietary approach should focus on preventing diverticulosis from progressing to diverticulitis. Contrary to popular belief, most people with diverticulosis can eat normally with minor adjustments.
Evolving Dietary Recommendations: What Changed?
Medical understanding of diverticulosis nutrition has significantly evolved. The table below shows how recommendations have shifted based on current evidence:
| Past Recommendations (Pre-2010s) | Current Evidence-Based Guidance |
|---|---|
| Avoid all seeds, nuts, and popcorn | These foods DON'T increase diverticulitis risk (Mayo Clinic, 2023) |
| Low-fiber diet during flare-ups | Gradual fiber reintroduction after acute phase (AGA Guidelines) |
| Strict food avoidance lists | Personalized approach focusing on overall dietary patterns |
| Emphasis on food restrictions | Focus on high-fiber foods that prevent complications |
Foods That May Aggravate Diverticulosis
While individual triggers vary, research identifies these dietary patterns associated with increased diverticulitis risk:
1. Low-Fiber Foods (Primary Concern)
Insufficient fiber contributes to constipation and increased colon pressure, potentially worsening diverticulosis. Limit these:
- Refined grains (white bread, pastries, regular pasta)
- Processed snacks (chips, crackers, cookies)
- Low-fiber cereals
- Processed meats (hot dogs, deli meats)
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recommends 25-30 grams of daily fiber to maintain regular bowel function and reduce complications. Most Americans consume only 15g daily.
2. High Red Meat Consumption
A 2021 study in Gut journal found that men consuming the most red meat had a 58% higher risk of diverticulitis compared to those with lowest intake. This association appears strongest with:
- Beef (especially processed varieties)
- Lamb
- Pork (particularly fatty cuts)
3. Individual Trigger Foods
Some people report specific food sensitivities during flare-ups. Common self-reported triggers include:
- High-fat fried foods
- Excessive caffeine
- Carbonated beverages
- Artificial sweeteners (sorbitol, mannitol)
Important context: These aren't universal triggers but may affect sensitive individuals. The American Gastroenterological Association emphasizes that trigger foods vary significantly between patients.
Practical Dietary Strategies for Diverticulosis Management
Instead of focusing solely on avoidance, build a protective dietary pattern:
Gradual Fiber Increase
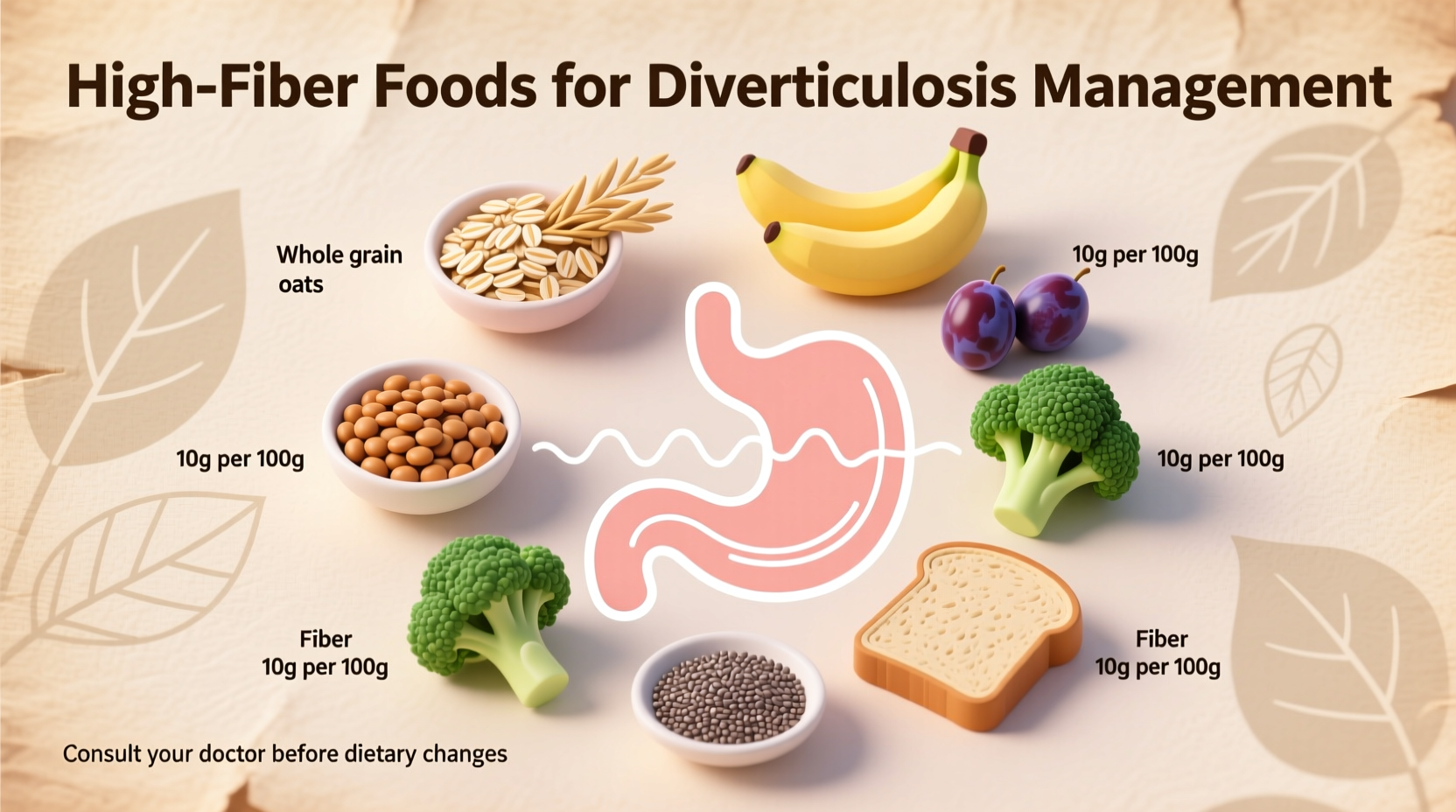
Rapidly increasing fiber can cause gas and bloating. Add 5g weekly until reaching 25-30g daily. Excellent sources include:
- Whole grains (oats, quinoa, brown rice)
- Legumes (lentils, black beans, chickpeas)
- Fruits with edible skins (apples, pears)
- Vegetables (broccoli, Brussels sprouts, carrots)
Hydration Is Critical
Fiber requires adequate water to function properly. Aim for at least 8 glasses daily. Dehydration combined with high fiber can worsen constipation.
Personalized Food Tracking
Keep a food and symptom diary for 2-4 weeks to identify your personal triggers. Note:
- What you ate
- Portion sizes
- Timing of consumption
- Any digestive symptoms
When to Consult Your Healthcare Provider
Dietary changes alone aren't sufficient if you experience:
- Severe abdominal pain (especially left lower quadrant)
- Unexplained fever
- Persistent changes in bowel habits
- Blood in stool
These symptoms may indicate diverticulitis requiring medical treatment. Never ignore persistent symptoms while attempting dietary management alone.
Evidence-Based Prevention Strategies
Research shows these approaches reduce diverticulitis risk:
- Maintaining healthy body weight (BMI 18.5-24.9)
- Regular physical activity (150 minutes moderate exercise weekly)
- Avoiding NSAIDs (ibuprofen, naproxen) which may increase risk
- Smoking cessation (smokers have 2x higher diverticulitis risk)
The Nurses' Health Study found that high dietary fiber combined with regular exercise reduced diverticulitis risk by 42% compared to low-fiber, sedentary lifestyles.
Building Your Diverticulosis-Friendly Plate
Create balanced meals using this simple framework:
- ½ plate non-starchy vegetables
- ¼ plate lean protein (fish, poultry, plant-based)
- ¼ plate whole grains or starchy vegetables
- Add healthy fats in moderation (olive oil, avocado)
Sample meal: Grilled salmon with roasted Brussels sprouts and quinoa, plus a side salad with olive oil dressing.
Common Misconceptions About Diverticulosis Diet
Let's clarify frequent points of confusion:
- Myth: Seeds and nuts get stuck in diverticula
- Fact: No scientific evidence supports this; these foods provide beneficial fiber
- Myth: You must follow a special diet with diverticulosis
- Fact: Most people need only moderate dietary adjustments focused on overall quality
- Myth: Diverticulosis always leads to diverticulitis
- Fact: Only 4-15% of people with diverticulosis develop diverticulitis
Working With Your Healthcare Team
For personalized guidance:
- Consult a registered dietitian specializing in gastrointestinal health
- Discuss fiber supplements if struggling to meet targets through food
- Ask about probiotic options that may support gut health
- Develop a symptom management plan for potential flare-ups
Remember that dietary management works best as part of comprehensive care including regular check-ups and appropriate screening.











 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4