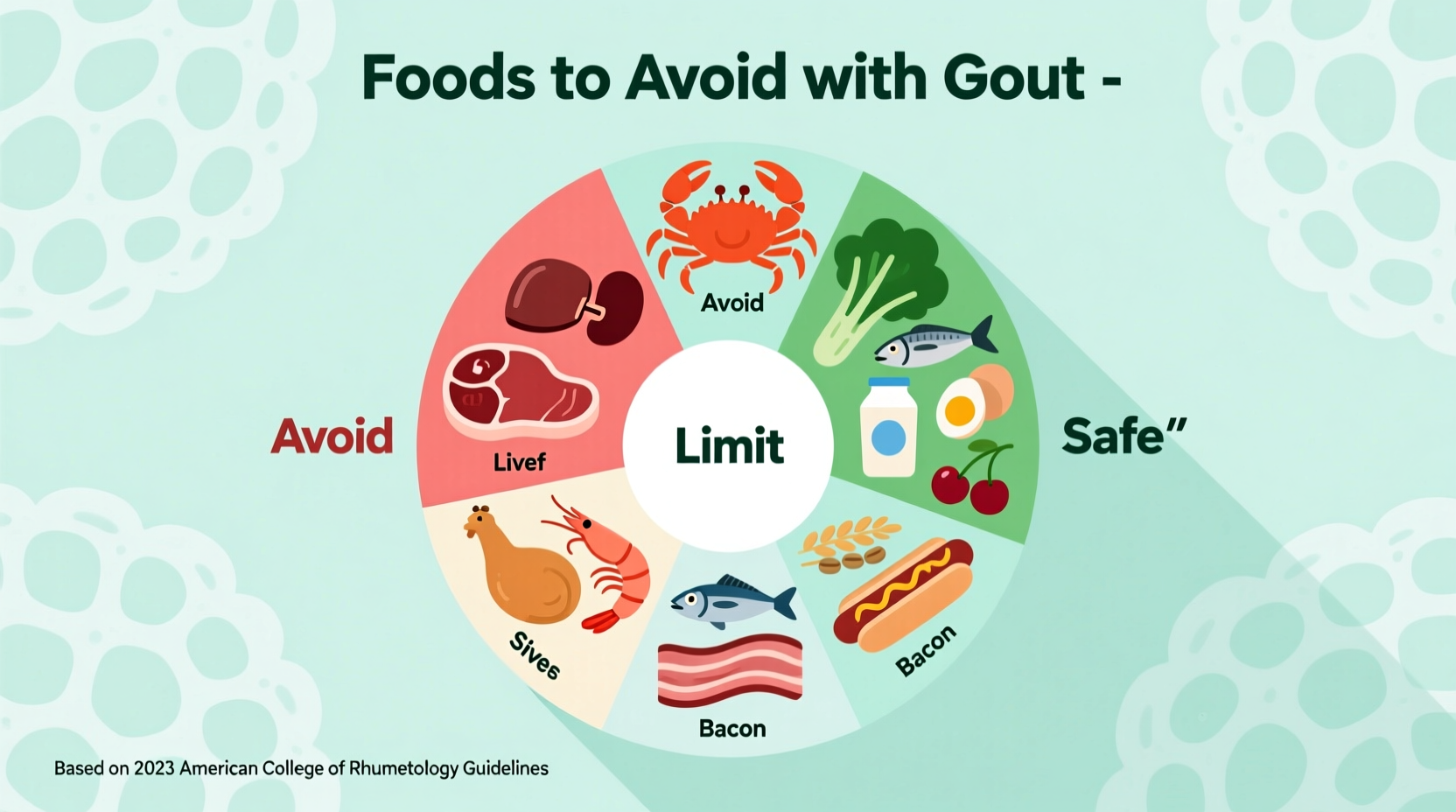
If you're managing gout, avoid high-purine foods like organ meats, certain seafood (anchovies, sardines, mussels), and excessive alcohol—especially beer. Also limit fructose-rich drinks, red meat, and foods with high-fructose corn syrup. These trigger uric acid buildup, causing painful flare-ups. Instead, prioritize low-fat dairy, vegetables, and moderate plant-based proteins.
Discover exactly which foods to eliminate from your diet and what to eat instead to reduce gout flare-ups. This guide delivers science-backed dietary strategies that rheumatologists recommend, helping you make informed choices without guesswork.
Understanding Gout and Dietary Triggers
Gout occurs when uric acid crystals accumulate in joints, causing intense pain and inflammation. Uric acid forms when your body breaks down purines—natural compounds found in certain foods. While your body produces purines naturally, consuming high-purine foods significantly increases uric acid levels, triggering flare-ups.
"Dietary management is crucial for gout patients," explains Dr. Hyon Choi, Director of the Clinical Epidemiology Research Unit at Massachusetts General Hospital. "While medications treat acute attacks, dietary changes reduce long-term flare frequency by 30-50%."

Foods That Trigger Gout Flare-Ups: The Science-Backed List
Not all high-purine foods affect everyone equally. However, research consistently identifies these categories as major triggers:
| Food Category | Purine Content (mg/100g) | Gout Risk Increase |
|---|---|---|
| Organ meats (liver, kidney) | 300-500 | 5x higher risk |
| Anchovies, sardines, mussels | 200-400 | 3.5x higher risk |
| Red meat (beef, lamb) | 100-200 | 1.4x higher risk |
| Beer (especially craft) | N/A (yeast content) | 2x higher risk |
Data sourced from the American College of Rheumatology and National Institute of Arthritis and Musculoskeletal and Skin Diseases. Note that individual responses vary—keep a food diary to identify your personal triggers.
Why Beer and Alcohol Worsen Gout
Alcohol interferes with uric acid excretion in two ways: beer contains high levels of purines from yeast, while all alcoholic beverages reduce kidney function. Research shows:
- Beer increases serum uric acid by 30% more than spirits
- Consuming 2+ beers daily raises gout risk by 200%
- Wine has less impact but should still be limited to 1-2 glasses
The Mayo Clinic recommends complete avoidance during flare-ups and strict moderation (1 drink max) during remission.
Hidden Triggers: Sugary Drinks and Processed Foods
Fructose metabolism directly increases uric acid production. Avoid:
- Sodas and fruit juices with high-fructose corn syrup
- Processed snacks containing corn syrup
- "Healthy" sweeteners like agave nectar
A 2022 Arthritis & Rheumatology study found that daily sugar-sweetened beverage consumption increased gout incidence by 85% compared to non-consumers.
Smart Swaps for Gout-Friendly Eating
You don't have to sacrifice flavor while managing gout. Try these evidence-based substitutions:
| Avoid | Try Instead | Why It Works |
|---|---|---|
| Beef stew | Mushroom & lentil stew | Plant proteins lower uric acid |
| Beer | Sparkling water with lime | No purines, promotes hydration |
| Soda | Tart cherry juice (unsweetened) | Anthocyanins reduce inflammation |
When Diet Alone Isn't Enough: Medical Considerations
Dietary changes typically reduce serum uric acid by 15-20%, but many patients require medication to reach the target level of <6 mg/dL. Consult your doctor if:
- You experience 2+ flare-ups per year
- Diet changes show no improvement after 3 months
- You develop tophi (uric acid crystal deposits)
The American College of Rheumatology emphasizes that combining medication with dietary management provides the best outcomes for chronic gout.
Implementing Your Gout Diet: Practical Steps
Start with these actionable strategies today:
- Week 1: Eliminate beer and sugary drinks completely
- Week 2: Replace red meat with poultry or tofu 3x weekly
- Week 3: Add 2 daily servings of low-fat dairy (milk, yogurt)
- Ongoing: Track food and symptoms using a dedicated app
Remember that hydration is critical—aim for 8-10 glasses of water daily to help flush uric acid. The Arthritis Foundation confirms that proper hydration reduces flare frequency by 25%.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4