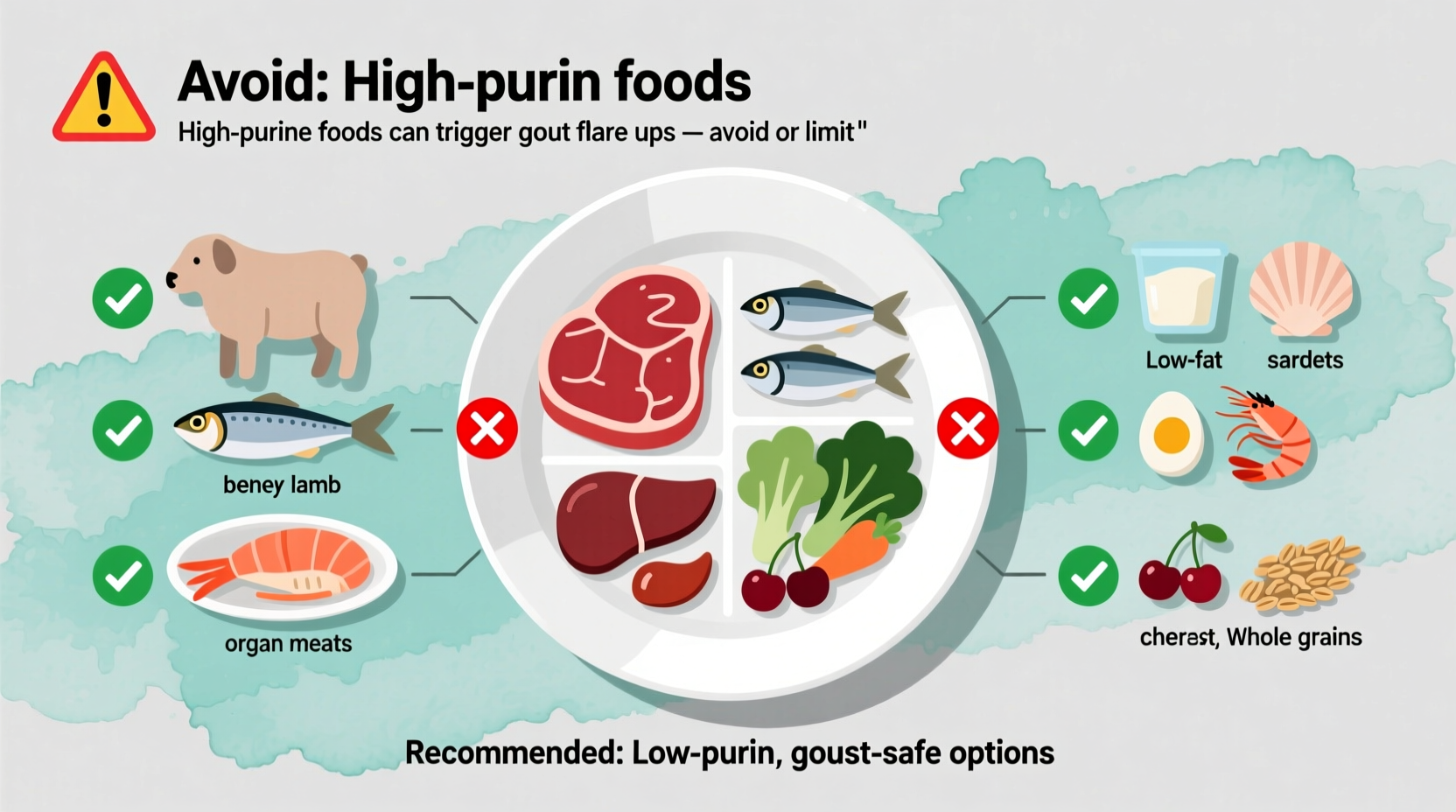
If you're managing gout, immediately avoid these top triggers: organ meats (liver, kidney), certain seafood (anchovies, sardines, mussels), red meat, game meats, beer, and sugary beverages. These high-purine foods significantly increase uric acid levels, triggering painful flare-ups. Research shows dietary changes can reduce gout attacks by up to 40% when combined with medical treatment.
Understanding which foods to avoid with gout isn't just about temporary relief—it's a crucial component of long-term management. Gout, the most common form of inflammatory arthritis, affects approximately 9 million Americans and occurs when excess uric acid forms needle-like crystals in your joints. While medication plays a vital role, dietary choices directly influence uric acid levels and flare frequency.
The Science Behind Gout and Diet
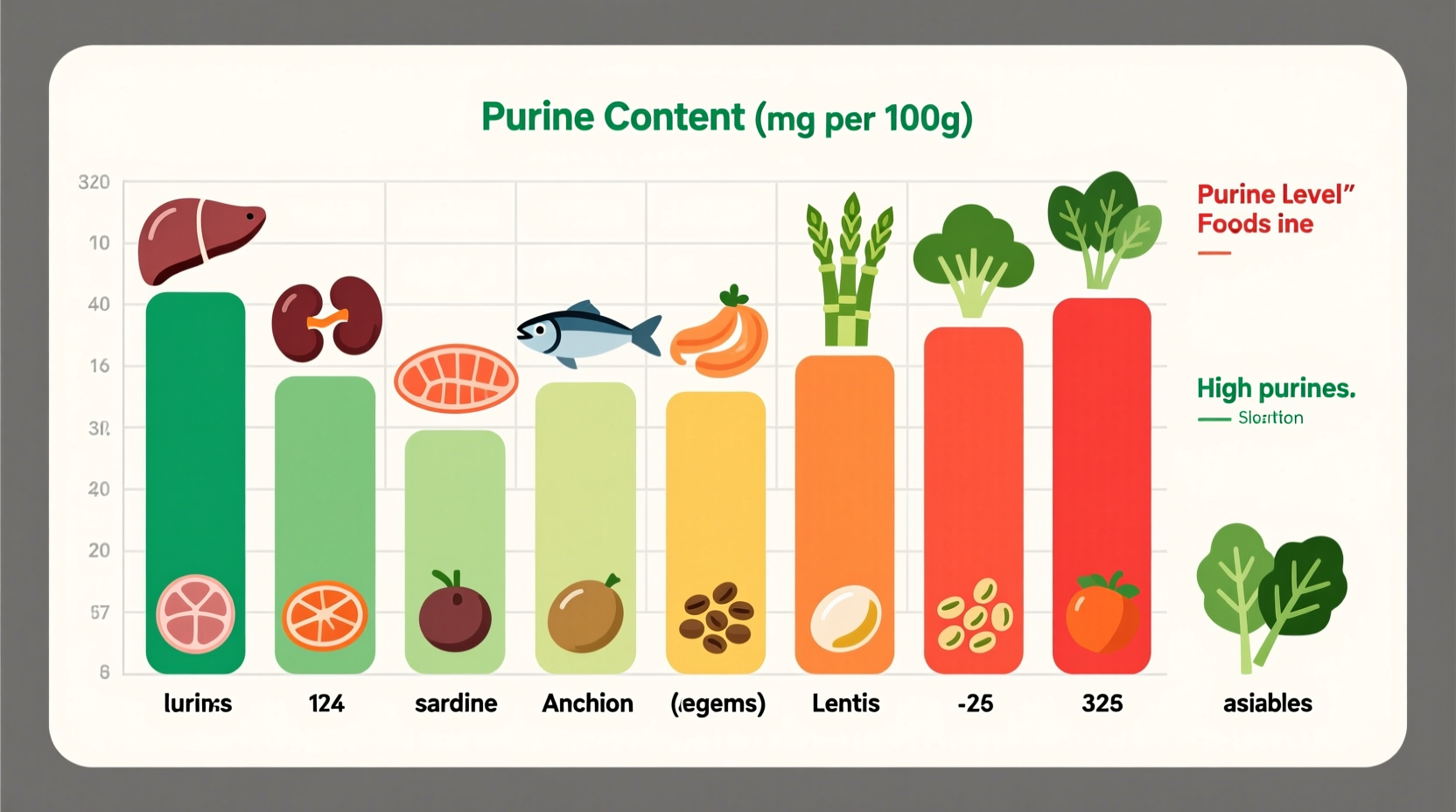
Uric acid forms when your body breaks down purines—natural compounds found in certain foods and produced by your body. When uric acid builds up in your bloodstream (hyperuricemia), it can crystallize in joints, causing the intense pain characteristic of gout attacks. According to the Centers for Disease Control and Prevention, dietary factors account for about 12% of serum uric acid levels, making food choices a significant controllable factor.
High-Purine Foods to Strictly Limit or Avoid
Medical research consistently identifies specific food categories that dramatically increase gout risk. The American College of Rheumatology recommends minimizing these high-purine foods:
Meat and Poultry Triggers
Organ meats represent the highest risk category, containing 200-500mg of purines per 3-ounce serving:
- Liver (beef, chicken, pork) - extremely high purine content
- Kidney and sweetbreads - should be completely avoided
- Red meats (beef, lamb, pork) - limit to 4-6 ounces maximum daily
- Game meats (venison, goose) - particularly problematic
A 2022 NIH study found that consuming just one additional serving of red meat daily increased gout risk by 21%.
Seafood Sensitivities
Certain seafood varieties contain exceptionally high purine levels that can trigger attacks within hours:
- Anchovies (800-1000mg purines per 3oz)
- Sardines (500-800mg)
- Mussels (500-700mg)
- Scallops (300-500mg)
- Tuna, trout, and haddock (moderate risk)
| Food Category | High-Risk Items | Safer Alternatives |
|---|---|---|
| Meats | Liver, kidney, game meats | Chicken breast, turkey |
| Seafood | Anchovies, sardines, mussels | Salmon, shrimp (in moderation) |
| Beverages | Beer, sugary sodas | Water, coffee, tart cherry juice |
| Plant Foods | None significantly problematic | All vegetables generally safe |
Beverage Triggers You Might Not Expect
What you drink affects gout almost as much as what you eat:
Alcohol's Double Impact
Beer poses the greatest risk due to both its purine content and alcohol's effect on uric acid excretion. Research published in Arthritis & Rheumatology shows that consuming just 1-2 beers daily increases gout attack risk by 69% compared to no alcohol. Spirits like vodka and whiskey present moderate risk, while moderate wine consumption shows minimal impact according to the same study.
Sugary Drinks and Fructose
Sweetened beverages containing high-fructose corn syrup significantly increase uric acid production. The Mayo Clinic reports that daily consumption of sugar-sweetened soft drinks increases gout risk by 85% compared to less than one serving monthly. Even 100% fruit juices with high fructose content should be limited.
Implementation Timeline: What to Expect
Dietary changes don't provide instant relief but follow a predictable pattern when consistently applied:
- Days 1-7: Eliminate all high-purine triggers; focus on hydration (8-10 glasses water daily)
- Weeks 2-4: Notice reduced frequency of minor joint discomfort; uric acid levels begin declining
- Month 2: Significant reduction in flare intensity when they occur
- Months 3-6: Most patients experience 30-40% fewer attacks with consistent dietary management
Remember that dietary changes work best alongside medication. The Arthritis Foundation emphasizes that while diet alone rarely controls gout completely, it significantly enhances medication effectiveness.
Practical Dining Strategies
Navigating social situations and restaurants becomes manageable with these evidence-based approaches:
- When ordering meat: Request lean cuts like chicken breast and ask for sauces on the side
- At seafood restaurants: Choose salmon or shrimp in moderation rather than high-risk options
- Reading labels: Check for high-fructose corn syrup in processed foods and beverages
- Meal timing: Spread protein intake throughout the day rather than large evening meals
When to Consult Your Healthcare Provider
Dietary management should complement—not replace—medical treatment. Consult your doctor if:
- You experience more than two gout attacks annually
- Pain persists beyond 7-10 days despite medication
- You develop tophi (uric acid crystal deposits under skin)
- Your uric acid levels remain above 6.0 mg/dL despite dietary changes
Remember that individual responses vary—what triggers one person's gout might not affect another. Keeping a detailed food and symptom journal helps identify your personal triggers more accurately than generalized lists.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4