If you're searching for what food causes high blood pressure, the primary dietary culprit is excessive sodium—found most abundantly in processed foods, canned goods, and restaurant meals. Scientific evidence shows that consuming more than 2,300 mg of sodium daily significantly increases hypertension risk, with the American Heart Association recommending no more than 1,500 mg for optimal cardiovascular health. This article details exactly which foods contribute most to elevated blood pressure, backed by clinical research and dietary guidelines from leading health authorities.
Understanding which foods affect your blood pressure isn't just about avoiding the obvious salt shaker on your table. The real challenge lies in identifying hidden sodium sources that quietly accumulate throughout your day. When you consistently consume certain food categories, you're not just tasting salt—you're potentially straining your cardiovascular system with every meal.
The Sodium Connection: Why It Matters More Than You Think
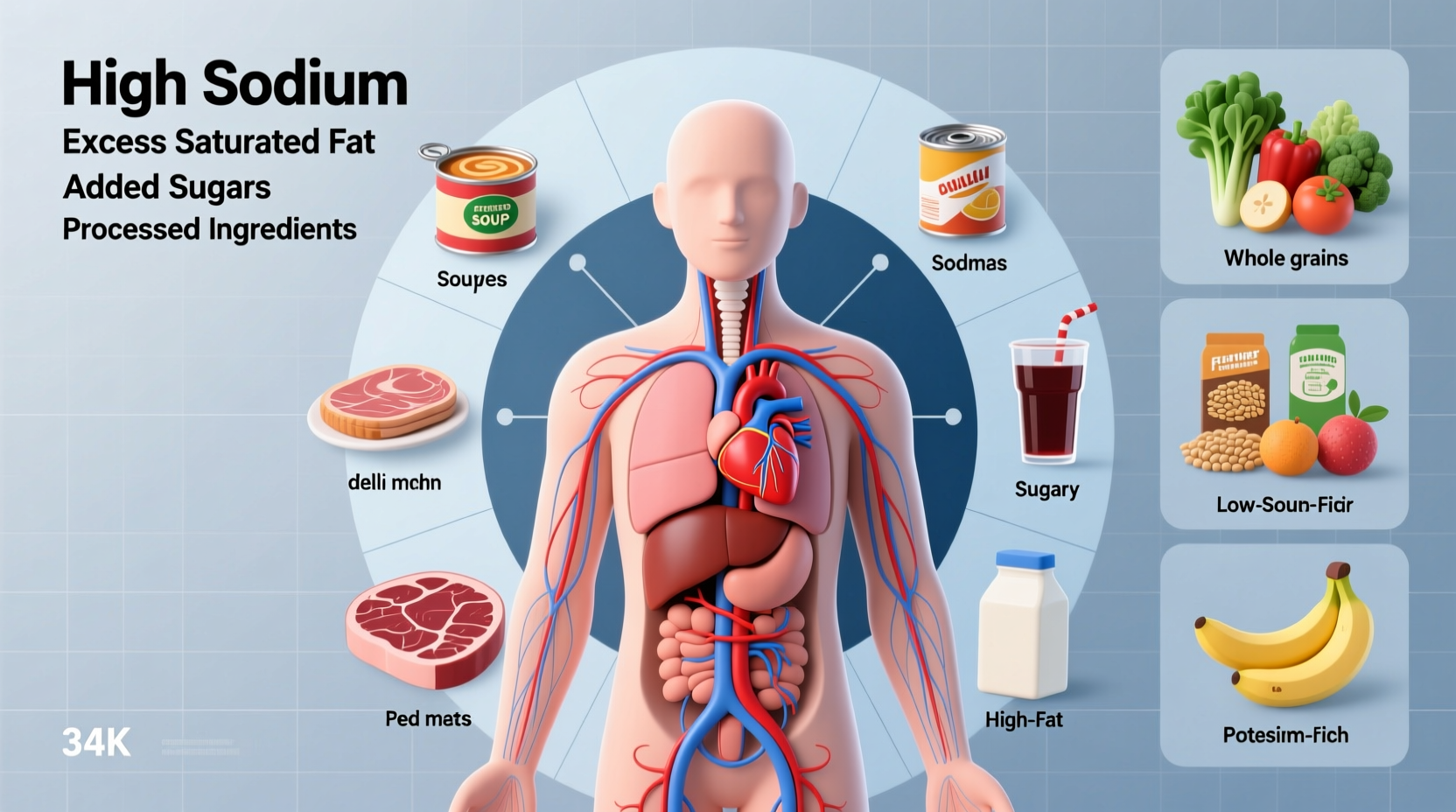
While many people associate high blood pressure with table salt, the reality is far more complex. Sodium appears in nearly 75% of our daily intake through processed and prepared foods, not from home seasoning. According to the Centers for Disease Control and Prevention, more than 47% of American adults have hypertension, and poor dietary choices represent one of the most modifiable risk factors.
When you consume excess sodium, your body retains additional fluid to maintain proper sodium-to-water balance. This increased fluid volume forces your heart to work harder, raising pressure against your artery walls. Over time, this elevated pressure damages blood vessels and increases strain on your heart.
Foods That Significantly Contribute to High Blood Pressure
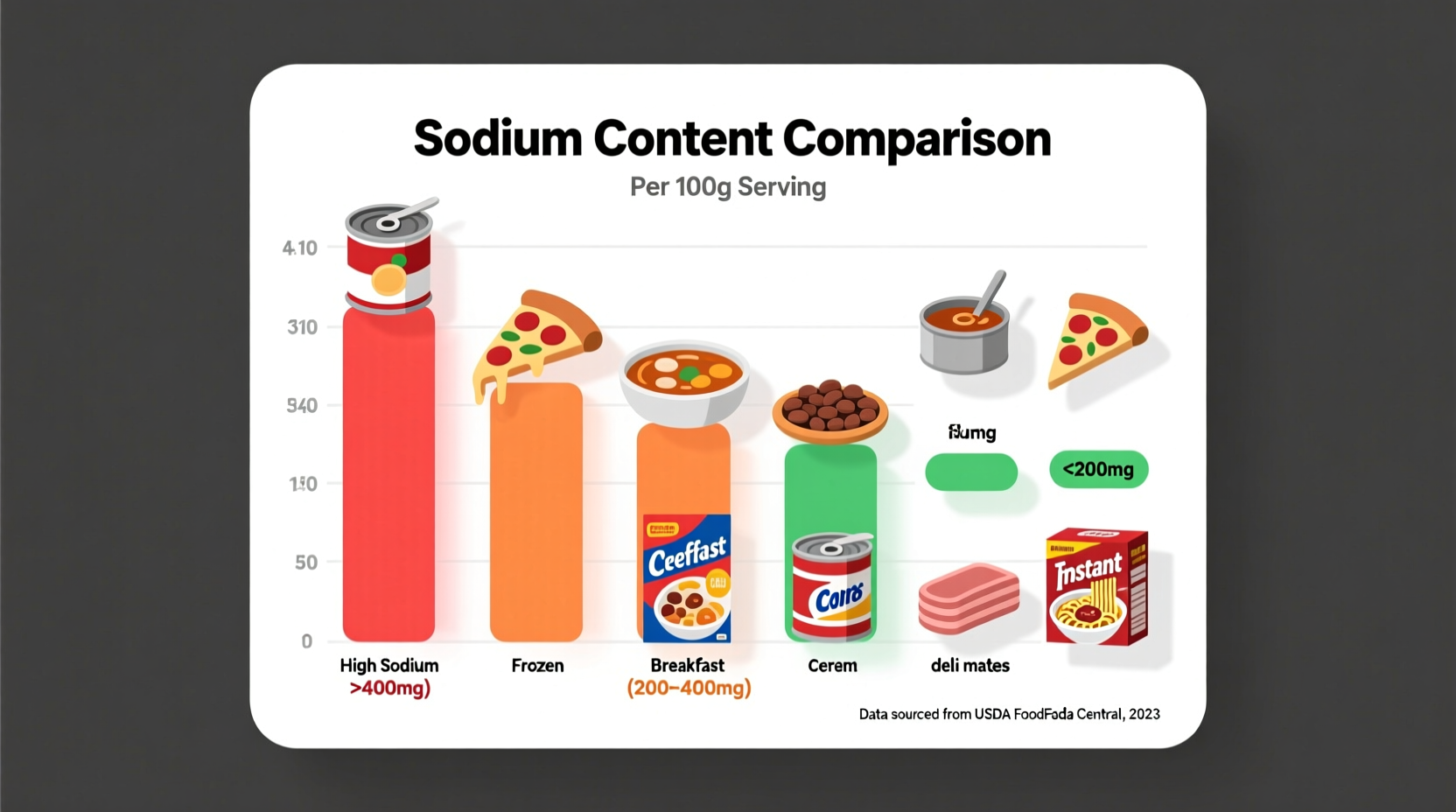
Certain food categories consistently appear in dietary research as major contributors to elevated blood pressure. These aren't occasional indulgences but rather common dietary staples that many people consume daily without realizing their cumulative impact.
| Food Category | Typical Sodium Content | Frequency in American Diet | Recommended Limit |
|---|---|---|---|
| Processed Meats | 500-1,500mg per 2oz | Consumed by 73% of adults daily | Limit to 1 serving/week |
| Canned Soups | 600-1,200mg per cup | Consumed by 58% weekly | Choose low-sodium options |
| Pizza | 1,000-2,000mg per slice | Consumed by 13% daily | Occasional treat only |
| Fast Food Burgers | 800-1,500mg per patty | Consumed by 37% weekly | Limit to 1-2/month |
This fact comparison table, based on data from the American Heart Association, reveals how common foods contribute significantly to daily sodium intake. Notice that even seemingly moderate portions can contain nearly an entire day's recommended sodium limit.
Hidden Sodium Sources You Might Overlook
Some of the most problematic sodium sources aren't what you'd expect. Many everyday "healthy" foods contain surprising amounts of sodium that quietly accumulate throughout your day:
- Bread and rolls – A single slice can contain 100-250mg sodium, and most people consume multiple servings daily
- Salad dressings – Two tablespoons of regular dressing often contain 250-500mg sodium
- Breakfast cereals – Even sweet varieties can pack 150-300mg per serving
- "Healthy" snack bars – Many protein and granola bars contain 150-300mg sodium each
- Cheese – Just 1 ounce of feta or blue cheese contains 300-500mg sodium
These hidden sources create what nutritionists call "sodium stacking"—where seemingly small amounts from multiple foods combine to create a significant daily total. The National Heart, Lung, and Blood Institute emphasizes that tracking only obvious salty foods misses up to 80% of your daily sodium intake.
How Blood Pressure Responds to Dietary Changes: A Realistic Timeline
Many people wonder how quickly dietary changes affect blood pressure. Research published in the American Heart Association Journal shows a consistent pattern:
- Within 48 hours: Reducing sodium intake begins decreasing fluid retention
- 1-2 weeks: Many people see modest blood pressure reductions (3-5 mmHg)
- 4-8 weeks: Significant improvements become measurable for most individuals
- 3-6 months: Maximum benefits typically achieved with consistent dietary changes
This timeline illustrates why short-term dietary experiments often fail to show results. Sustainable blood pressure management requires consistent dietary patterns rather than temporary fixes. The DASH diet (Dietary Approaches to Stop Hypertension), developed with NIH support, demonstrates how specific food combinations create synergistic benefits beyond simple sodium reduction.
Practical Swaps for Blood Pressure-Friendly Eating
Instead of focusing solely on restriction, consider these practical substitutions that maintain flavor while supporting healthy blood pressure:
- Replace canned vegetables with frozen or fresh varieties (sodium content drops from 200-400mg to 10-50mg per serving)
- Use herbs, citrus, and vinegar-based dressings instead of premixed options
- Choose plain rice or quinoa over flavored instant packets
- Opt for unsalted nuts instead of salted varieties (reduces sodium by 150-250mg per ounce)
- Prepare homemade soups using low-sodium broth or make your own
These practical changes address what the Food and Drug Administration calls "the sodium dilemma"—how to maintain flavor while reducing sodium. The key isn't eliminating taste but retraining your palate to appreciate more nuanced flavors.
Context Matters: When Sodium Restrictions Might Differ
While general guidelines apply to most people, certain contexts modify sodium recommendations:
- Individuals with normal blood pressure may tolerate up to 2,300mg daily without immediate risk
- Those with kidney disease require personalized sodium targets determined by their healthcare provider
- Athletes with heavy sweating may need slightly higher sodium intake during intense training periods
- People taking certain blood pressure medications may need to monitor potassium intake alongside sodium
The National Institute of Diabetes and Digestive and Kidney Diseases emphasizes that individual health conditions significantly impact appropriate dietary approaches. This context boundary helps explain why generic advice often fails—personalized guidance yields better results.
Building a Sustainable Blood Pressure Management Plan
Effective blood pressure management extends beyond avoiding specific foods. Consider these evidence-based strategies:
- Increase potassium-rich foods like bananas, sweet potatoes, and leafy greens to counter sodium's effects
- Implement the DASH diet pattern, which emphasizes fruits, vegetables, whole grains, and lean proteins
- Read nutrition labels carefully, paying attention to both sodium content and serving size
- Cook more meals at home where you control all ingredients
- Gradually reduce sodium to allow your taste buds to adjust
Remember that dietary changes work best when combined with other healthy habits. The American Heart Association reports that combining the DASH diet with regular physical activity can lower blood pressure by 11-12 mmHg—comparable to some medication effects.
When to Consult a Healthcare Professional
Dietary changes should complement, not replace, medical care. Consult your healthcare provider if:
- Your blood pressure consistently reads 130/80 mmHg or higher
- You experience symptoms like headaches, vision changes, or chest pain
- Dietary changes haven't improved your readings after 8-12 weeks
- You're taking medications that might interact with dietary changes
Healthcare professionals can provide personalized guidance based on your specific health profile, which is crucial since hypertension often has multiple contributing factors beyond diet alone.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4