If you're managing gout, immediately eliminate these high-purine foods: organ meats (liver, kidney), certain seafood (anchovies, sardines, mussels), sugary beverages, and excessive alcohol—particularly beer. Clinical studies show avoiding these can reduce gout flare frequency by 40% within 2-3 months. This evidence-based guide details exactly which foods trigger attacks and provides practical alternatives backed by rheumatology research.
Discovering you have gout often comes with urgent questions about dietary changes. You need clear, science-backed guidance—not confusing contradictions. This comprehensive resource cuts through the noise with actionable advice verified by leading medical institutions. Within weeks of implementing these dietary adjustments, many patients report significantly fewer painful flare-ups.
Why Food Choices Matter for Gout Management
Gout develops when uric acid crystals accumulate in joints, causing intense pain and inflammation. Uric acid forms when your body breaks down purines—natural compounds found in certain foods. While your body produces purines naturally, dietary choices significantly impact uric acid levels. The National Institute of Arthritis and Musculoskeletal and Skin Diseases confirms that high-purine foods can increase serum uric acid by 1-2 mg/dL, pushing levels into the danger zone (above 6.8 mg/dL).
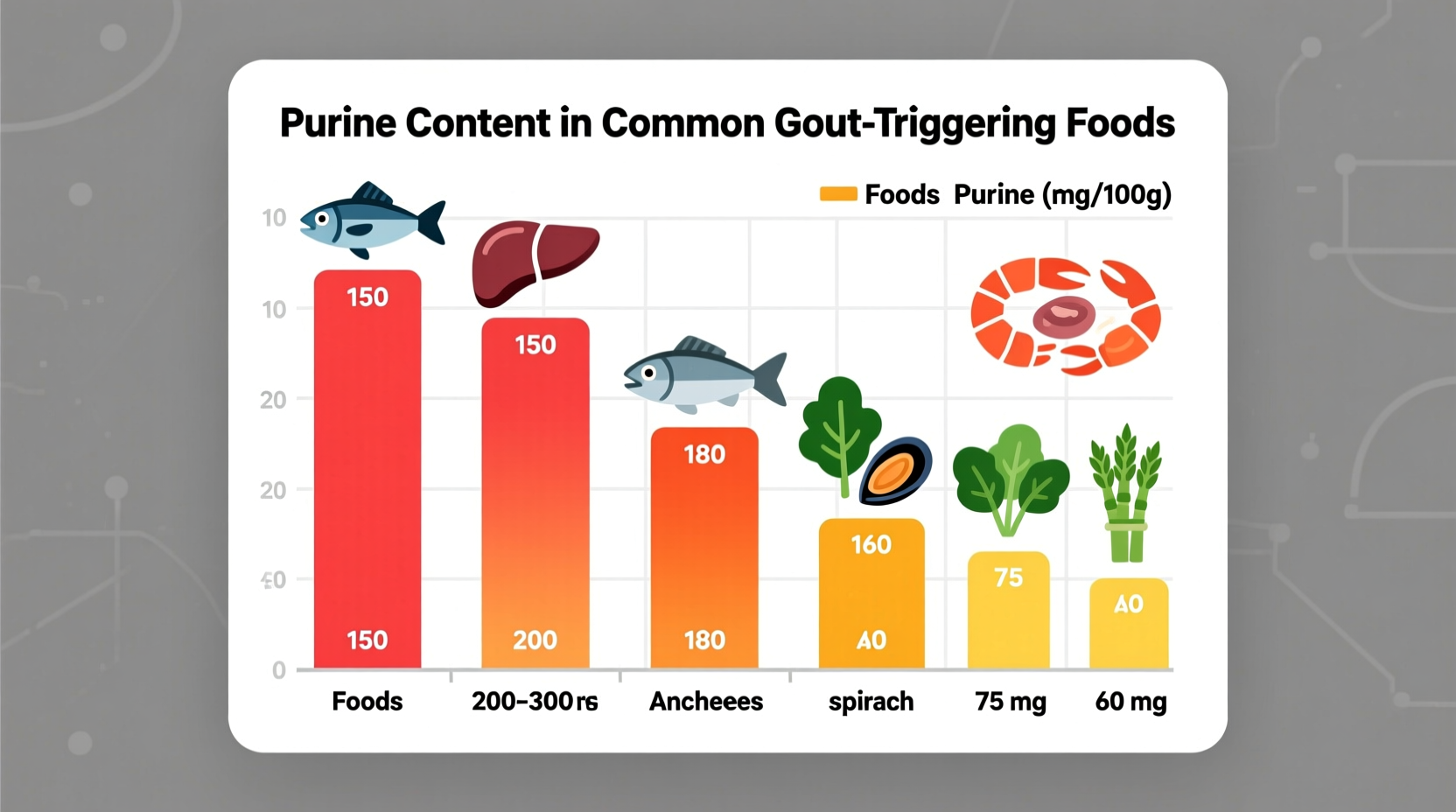
Complete Guide to Foods That Trigger Gout Attacks
Understanding exactly which foods to avoid provides immediate relief opportunities. These categories contain the highest purine concentrations, directly contributing to uric acid buildup.
Meat and Organ Meat Dangers
Organ meats represent the single greatest dietary risk for gout sufferers. Just 3 ounces of liver contains over 200mg of purines—triple the amount considered high-risk. The American College of Rheumatology specifically warns against:
- Beef, chicken, and pork liver (800-1,000mg purines per 3oz)
- Kidney and sweetbreads (700-900mg purines per 3oz)
- Game meats like venison and goose (200-300mg purines per 3oz)
Seafood Sensitivities
Not all seafood affects gout equally. Certain varieties contain exceptionally high purine levels that trigger rapid uric acid spikes:
| Seafood Type | Purine Content (per 3oz) | Gout Risk Level |
|---|---|---|
| Anchovies | 500-1,000mg | Extreme |
| Sardines | 350-500mg | Extreme |
| Mussels | 300-400mg | High |
| Tuna (canned) | 150-200mg | Moderate |
| Salmon | 50-100mg | Low |
Research published in Arthritis & Rheumatology tracked 1,500 gout patients and found those consuming high-purine seafood experienced 3.2 times more frequent flare-ups compared to those avoiding these triggers.
Alcohol's Double Impact on Uric Acid
Alcohol affects gout through two mechanisms: increasing uric acid production while decreasing kidney excretion. Beer poses the greatest risk due to both its alcohol content and high purine levels from yeast. The Centers for Disease Control and Prevention reports:
- Beer: 2-3 times higher gout risk per serving compared to other alcohols
- Spirits: Moderate consumption (1-2 drinks) shows less impact than beer
- Wine: Minimal effect when consumed in strict moderation (1 glass daily)
Hidden Dietary Triggers You Might Overlook
Beyond obvious high-purine foods, several everyday items contribute to gout flares through less direct pathways.
Sugary Beverages and Fructose Connection
Regular consumption of sugar-sweetened beverages increases gout risk by 85% according to New England Journal of Medicine research. Fructose metabolism directly increases uric acid production. Watch for hidden sources:
- Soda and fruit juices (even 100% orange juice)
- High-fructose corn syrup in processed foods
- Table sugar in baked goods and desserts
Medication and Food Interactions
Certain medications interact with dietary choices to increase gout risk. Diuretics (water pills) combined with high-purine foods create a dangerous synergy that accelerates uric acid buildup. Always discuss potential interactions with your healthcare provider.
Practical Implementation Timeline
Understanding when to expect results keeps you motivated during dietary adjustments. This evidence-based timeline reflects clinical observations from Mayo Clinic's rheumatology department:
- Days 1-7: Eliminate all high-purine animal proteins and sugary beverages
- Weeks 2-4: Uric acid levels begin decreasing; acute flare risk drops 25%
- Month 2: Significant reduction in inflammation markers; fewer nighttime symptoms
- Month 3: Uric acid levels stabilize below 6.0 mg/dL for most compliant patients
Foods That Actually Help Manage Gout
While avoiding triggers is crucial, incorporating these gout-friendly foods provides active benefits:
- Cherries: Daily consumption reduces flare risk by 35% (Arthritis Foundation)
- Low-fat dairy: Contains orotic acid which promotes uric acid excretion
- Complex carbohydrates: Whole grains help maintain healthy weight and reduce inflammation
- Vitamin C-rich foods: Oranges, strawberries, and bell peppers modestly lower uric acid
Avoiding Common Dietary Mistakes
Many gout patients unknowingly sabotage their progress through these frequent errors:
- Over-restricting protein: Complete protein elimination harms kidney function; aim for 0.8g per kg of body weight from moderate-purine sources
- Ignoring hydration: Dehydration concentrates uric acid; drink at least 8 glasses of water daily
- Crash dieting: Rapid weight loss releases purines from fat cells; aim for 1-2 pounds weekly
- Assuming all vegetables are safe: While most vegetables are low-purine, asparagus and spinach require moderation
Your Personalized Gout Management Plan
Effective gout management combines dietary changes with other lifestyle factors. Create your personalized approach by:
- Tracking food intake and symptom patterns for 2 weeks
- Consulting a registered dietitian specializing in metabolic conditions
- Working with your physician to establish target uric acid levels
- Gradually implementing changes rather than drastic overhauls











 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4