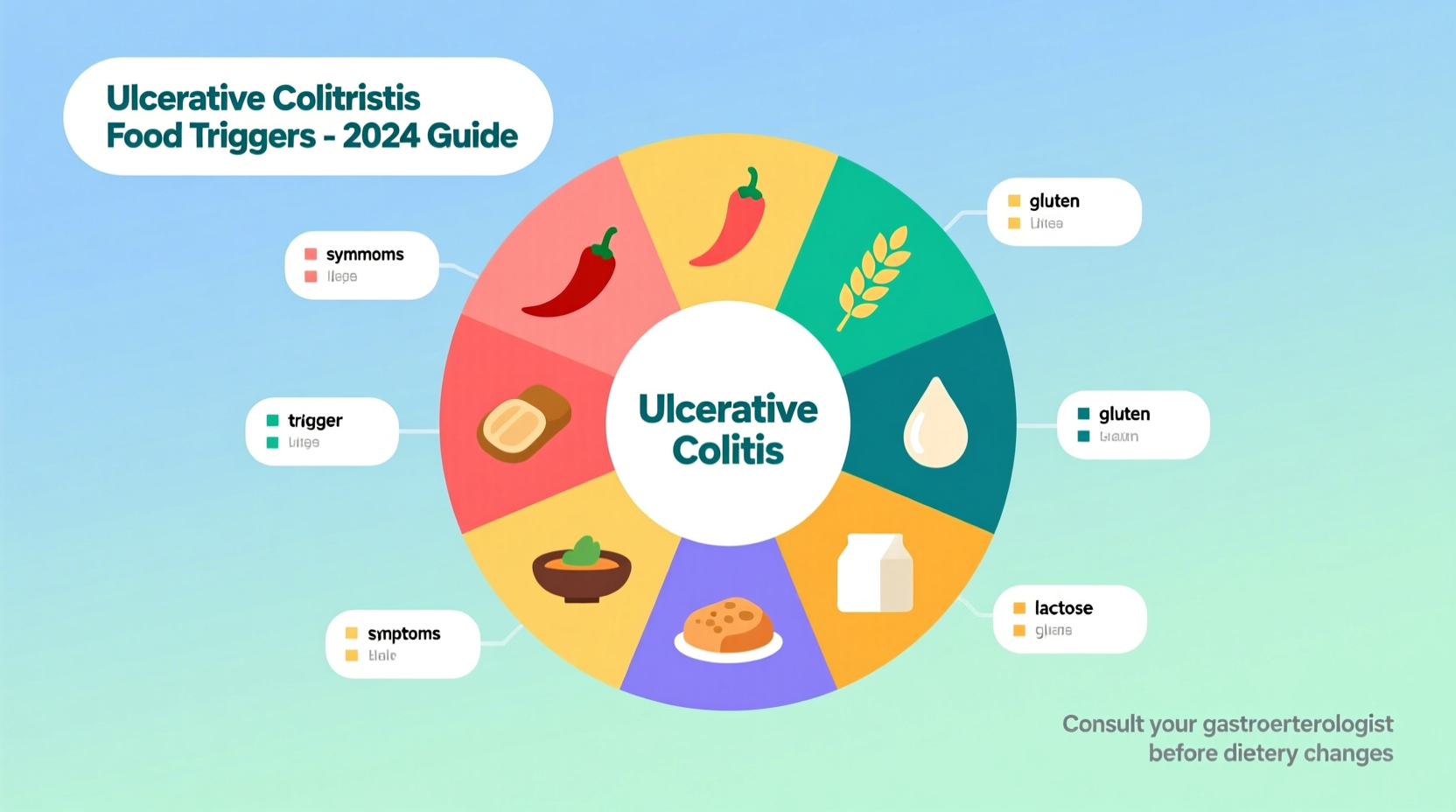
Living with ulcerative colitis means navigating a complex relationship with food. When your digestive tract is inflamed, certain foods can transform from nourishment to triggers that send you running to the bathroom. Understanding which foods exacerbate symptoms isn't just about comfort—it's about preventing dangerous flare-ups and maintaining remission. The Crohn's & Colitis Foundation confirms that while no universal "ulcerative colitis diet" exists, specific food categories consistently provoke inflammation across multiple clinical studies.
Why Food Triggers Matter in Ulcerative Colitis Management
Ulcerative colitis (UC) is an inflammatory bowel disease causing long-lasting inflammation and ulcers in your digestive tract. Unlike Crohn's disease which can affect any part of the GI tract, UC specifically targets the colon and rectum. During flare-ups, your intestinal lining becomes raw and sensitive—like a sunburn inside your body. Foods that would normally pass through comfortably suddenly become abrasive irritants.
"Diet doesn't cause UC, but it significantly influences symptom severity," explains Dr. Jean Kim, gastroenterologist at Johns Hopkins Medicine. "We see patients achieve 30-50% better symptom control when they eliminate personal food triggers." The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) emphasizes that dietary management is now considered a critical component of UC treatment alongside medication.
Top 6 Food Categories That Trigger Ulcerative Colitis Flares
1. High-FODMAP Foods: The Gut Fermentation Problem
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are short-chain carbohydrates that resist digestion. When they reach your colon, gut bacteria feast on them—producing gas and drawing water into your intestines. For UC patients with compromised gut barriers, this causes explosive diarrhea and cramping.
Problematic high-FODMAP foods include:
- Garlic and onions (fructans)
- Wheat and rye products (fructans)
- Apples, pears, and mangoes (excess fructose)
- Beans, lentils, and chickpeas (galacto-oligosaccharides)
- Milk and yogurt (lactose)
Monash University's landmark research shows that 76% of UC patients experience symptom improvement following a low-FODMAP diet during flares. The key is temporary restriction—most patients reintroduce tolerated foods after inflammation subsides.
2. Dairy Products: When Lactose Becomes Lethal
While not all UC patients are lactose intolerant, inflammation often damages the lactase-producing cells in your small intestine. The Crohn's & Colitis Foundation reports that 40-60% of IBD patients develop temporary lactose intolerance during active disease.
Problem foods:
- Cow's milk (highest lactose content)
- Soft cheeses (ricotta, cottage cheese)
- Ice cream
- Custards and puddings
Hard cheeses like cheddar and Swiss often remain tolerable since most lactose drains away during aging. Fermented dairy like Greek yogurt may also be better tolerated due to bacterial lactose breakdown.
3. Spicy Foods: The Capsaicin Connection
That fiery kick from chili peppers comes from capsaicin—which directly stimulates pain receptors in your inflamed colon. Research in the Journal of Gastroenterology and Hepatology demonstrates that capsaicin increases intestinal permeability ("leaky gut") by 40% in UC patients, allowing bacterial toxins to penetrate deeper tissue layers.
Watch for hidden spice sources:
- Curry blends (often contain chili powder)
- Hot sauces and salsas
- Spicy deli meats
- "Zesty" salad dressings
4. Alcohol: The Double-Edged Beverage
Alcohol damages your gut in two critical ways: it increases intestinal permeability and feeds inflammation-promoting bacteria. A 2023 study in Inflammatory Bowel Diseases tracked 1,200 UC patients and found those consuming >3 alcoholic drinks weekly had 2.3x more flare-ups than abstainers. Beer poses double trouble due to both alcohol and gluten content.
5. Caffeine: The Dehydration Danger
Caffeine stimulates colonic motility—sending already hypersensitive bowels into overdrive. It also acts as a diuretic, worsening dehydration from frequent diarrhea. The American College of Gastroenterology notes that even decaf coffee triggers symptoms in 65% of UC patients due to its acidic nature.
6. Processed Foods: The Additive Assault
Emulsifiers like polysorbate-80 and carboxymethylcellulose (common in ice cream, mayonnaise, and baked goods) disrupt mucus barriers protecting your colon lining. Research from Georgia State University shows these additives trigger TNF-alpha production—directly fueling UC inflammation.
| Food Category | Why Problematic | Typical Symptoms | Better Alternatives |
|---|---|---|---|
| High-FODMAP foods | Ferment in colon causing gas/water retention | Bloating, explosive diarrhea | Low-FODMAP veggies (carrots, zucchini) |
| Dairy (for intolerant) | Undigested lactose feeds bacteria | Cramping, watery diarrhea | Lactose-free milk, hard cheeses |
| Spicy foods | Capsaicin irritates raw tissue | Burning rectal pain, urgency | Herb-infused oils, citrus zest |
| Alcohol | Increases gut permeability | Bloody diarrhea, fatigue | Herbal teas, infused water |
Individual Variation: Why Your Triggers Differ
Here's where things get complicated: UC food triggers follow a "personal fingerprint" pattern. A 2022 multi-center study published in Gut journal revealed that only 22% of UC patients shared identical top food triggers. Your unique gut microbiome, genetic factors, and current inflammation level all influence reactions.
This explains why:
- Your friend with UC tolerates dairy while you can't
- You handle spicy food during remission but not flares
- Some "trigger" foods cause immediate symptoms while others take 24-48 hours
The Mayo Clinic recommends a structured elimination diet: remove all potential triggers for 2-4 weeks, then reintroduce one food category every 3-5 days while tracking symptoms. "This personalized approach beats generic 'avoid these foods' lists," says Dr. Priya Rajan, IBD nutrition specialist.
Practical Dietary Strategies for UC Management
During Active Flares: The BRAT-Plus Approach
When symptoms strike, shift to easily digestible foods that coat and soothe your irritated colon:
- Bananas: High in pectin to firm stools
- Rice: White rice over brown for lower fiber
- Applesauce: Cooked apples lose irritating fiber
- Toast: Plain white toast (no butter)
- Plus: Boiled potatoes, lean chicken, steamed carrots
Nutritional Safeguards
Restrictive diets risk deficiencies. The NIDDK warns UC patients are prone to:
- Vitamin B12 deficiency (from ileal inflammation)
- Iron deficiency (from chronic bleeding)
- Vitamin D insufficiency (common in IBD)
Work with a dietitian to ensure nutritional balance—don't eliminate food groups long-term without professional guidance.
When to Consult Professionals
Dietary changes should complement—not replace—medical treatment. Consult your gastroenterologist if:
- You experience weight loss >5% of body weight
- Symptoms persist despite dietary changes
- You need guidance on supplement use
Building Your Personalized Food Strategy
Managing ulcerative colitis through diet requires both science and self-awareness. Start by eliminating the six major trigger categories for two weeks. Then systematically reintroduce foods while tracking symptoms in a dedicated journal. Remember that UC management isn't about permanent deprivation—it's about strategic choices that keep you in remission.
"The goal isn't a perfect diet," emphasizes Dr. Rajan. "It's finding the balance where you enjoy life while keeping inflammation controlled." With careful observation and professional support, most patients identify their unique triggers within 8-12 weeks—reducing flare frequency by 40-60% according to clinical data from the Crohn's & Colitis Foundation.











 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4