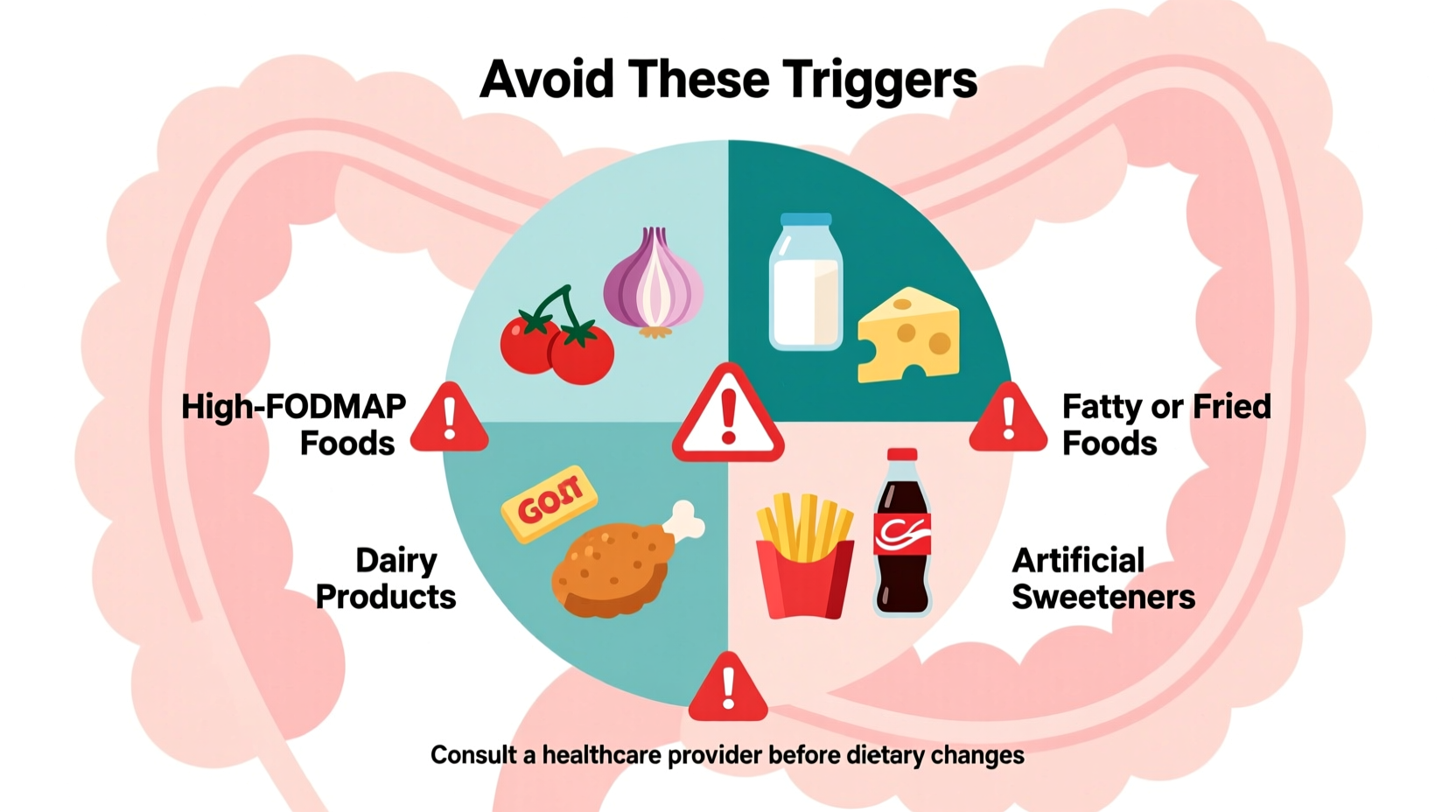
Based on clinical research and gastroenterology guidelines, the worst foods for IBS include high-FODMAP items like onions, garlic, wheat, dairy products containing lactose, certain fruits (apples, pears), artificial sweeteners (sorbitol, mannitol), and carbonated beverages. These trigger symptoms in 75% of IBS patients by causing gas, bloating, and irregular bowel movements.
If you're struggling with irritable bowel syndrome, identifying dietary triggers is your most effective management strategy. Research shows that eliminating specific problematic foods reduces symptoms in 50-80% of IBS cases. This evidence-based guide reveals exactly which foods exacerbate IBS symptoms and why, plus practical alternatives you can implement immediately.
Understanding IBS Food Triggers: The Science Behind Symptoms
IBS affects approximately 10-15% of the global population, with dietary factors playing a crucial role in symptom management. When certain foods reach your small intestine undigested, they ferment and draw water into the gut through osmosis. This process creates gas, distension, and triggers abnormal contractions in sensitive intestinal nerves.
"The low-FODMAP diet remains the gold standard for dietary management of IBS," explains Dr. William Chey, Director of the University of Michigan's Gastrointestinal Motility Program. "By reducing fermentable carbohydrates, we see significant symptom improvement in the majority of patients within 2-6 weeks."
Top IBS Trigger Foods: Evidence-Based Analysis
Based on clinical studies published in Gastroenterology and guidelines from the International Foundation for Gastrointestinal Disorders, these foods consistently provoke symptoms:
| Food Category | Specific Triggers | Why They Cause Problems | Research Support Level |
|---|---|---|---|
| High-FODMAP Vegetables | Onions, garlic, cauliflower, mushrooms | Fructans and GOS cause rapid fermentation and gas production | ★★★★★ (Multiple RCTs) |
| Dairy Products | Milk, soft cheeses, ice cream | Lactose intolerance affects 65% of IBS patients | ★★★★☆ (Strong clinical evidence) |
| Artificial Sweeteners | Sorbitol, mannitol, xylitol | Osmotic effect draws water into bowel causing diarrhea | ★★★★☆ (Consistent patient reports) |
| High-Fat Foods | Fried foods, fatty meats, creamy sauces | Accelerates colonic contractions triggering diarrhea | ★★★☆☆ (Moderate evidence) |
| Certain Fruits | Apples, pears, mangoes, watermelon | Excess fructose and sorbitol overwhelm digestive capacity | ★★★★★ (Multiple RCTs) |
Context Matters: When Trigger Foods Might Be Tolerable
Not all IBS patients react to the same triggers. Your tolerance depends on several factors:
- IBS Subtype: Diarrhea-predominant (IBS-D) patients typically react more strongly to fatty foods and caffeine, while constipation-predominant (IBS-C) patients may tolerate these better but react to low-fiber foods
- Portion Size: Small amounts of garlic (1/8 teaspoon) may be tolerable when larger quantities trigger symptoms
- Food Combination: Eating high-FODMAP foods with protein or fat can slow digestion and reduce symptoms
- Individual Thresholds: Research shows symptom thresholds vary significantly between patients (source: National Institute of Diabetes and Digestive and Kidney Diseases)
Implementing an Effective IBS Diet Strategy
Successful dietary management requires a structured approach rather than random elimination:
Phase 1: Elimination (4-6 weeks)
Remove all major trigger foods simultaneously. The low-FODMAP diet developed at Monash University provides the most evidence-based framework. During this phase, focus on:
- Low-FODMAP vegetables: carrots, zucchini, bell peppers, spinach
- Safe proteins: eggs, tofu, chicken, fish
- Low-FODMAP fruits: strawberries, blueberries, oranges
- Lactose-free dairy alternatives
Phase 2: Reintroduction (8-12 weeks)
Systematically reintroduce potential triggers one at a time, monitoring symptoms. The Monash University FODMAP app provides detailed reintroduction protocols. This phase reveals your personal tolerance thresholds.
Phase 3: Personalization (Ongoing)
Create your customized long-term diet based on reintroduction results. Most patients can eventually tolerate 50-75% of previously eliminated foods at appropriate portions.
Common Misconceptions About IBS and Diet
Several widespread beliefs about IBS diets lack scientific support:
- "Gluten is the main problem": Research shows only 25% of IBS patients actually react to gluten specifically; most react to fructans in wheat (source: Mayo Clinic)
- "Dairy elimination is always necessary": Lactose intolerance affects only 65% of IBS patients; hard cheeses and fermented dairy are often tolerated
- "All fiber helps IBS": Insoluble fiber (wheat bran) worsens symptoms for many, while soluble fiber (psyllium) helps 70% of patients
Practical Implementation Tips
Make dietary changes sustainable with these evidence-based strategies:
- Use the Monash University FODMAP app to identify safe portions when eating out
- Keep a detailed food-symptom journal tracking not just what you eat but timing and stress levels
- When cooking, replace garlic and onion with infused oils (garlic-infused oil contains no FODMAPs)
- Choose lactose-free alternatives that contain added calcium and vitamin D
- Gradually increase soluble fiber to 10-15g daily using psyllium husk
When Diet Isn't Enough: Comprehensive Management
Dietary changes work for 70-80% of IBS patients, but complete management often requires additional approaches:
- Stress management: Cognitive behavioral therapy reduces symptom severity by 40-60% (source: International Foundation for Gastrointestinal Disorders)
- Probiotics: Specific strains like Bifidobacterium infantis show moderate benefit for bloating and pain
- Medication: For persistent symptoms, medications like eluxadoline (IBS-D) or linaclotide (IBS-C) may be appropriate
Long-Term Dietary Balance
While eliminating trigger foods provides relief, maintaining nutritional balance is crucial. Research shows IBS patients often develop unnecessary food restrictions leading to nutrient deficiencies. Work with a registered dietitian to ensure your modified diet includes adequate:
- Calcium and vitamin D (especially if avoiding dairy)
- Fiber from tolerated sources
- B vitamins often found in whole grains
- Essential fatty acids










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4