Understanding Food Triggers for Digestive Distress
When your digestive system reacts with unexpected urgency, identifying the culprit in your diet becomes essential. Diarrhea affects millions daily, often triggered by specific foods that disrupt normal bowel function. This guide helps you recognize common dietary triggers, understand why they cause problems, and implement practical strategies to maintain digestive comfort.Top Food Categories That Cause Diarrhea
Dairy Products and Lactose Intolerance
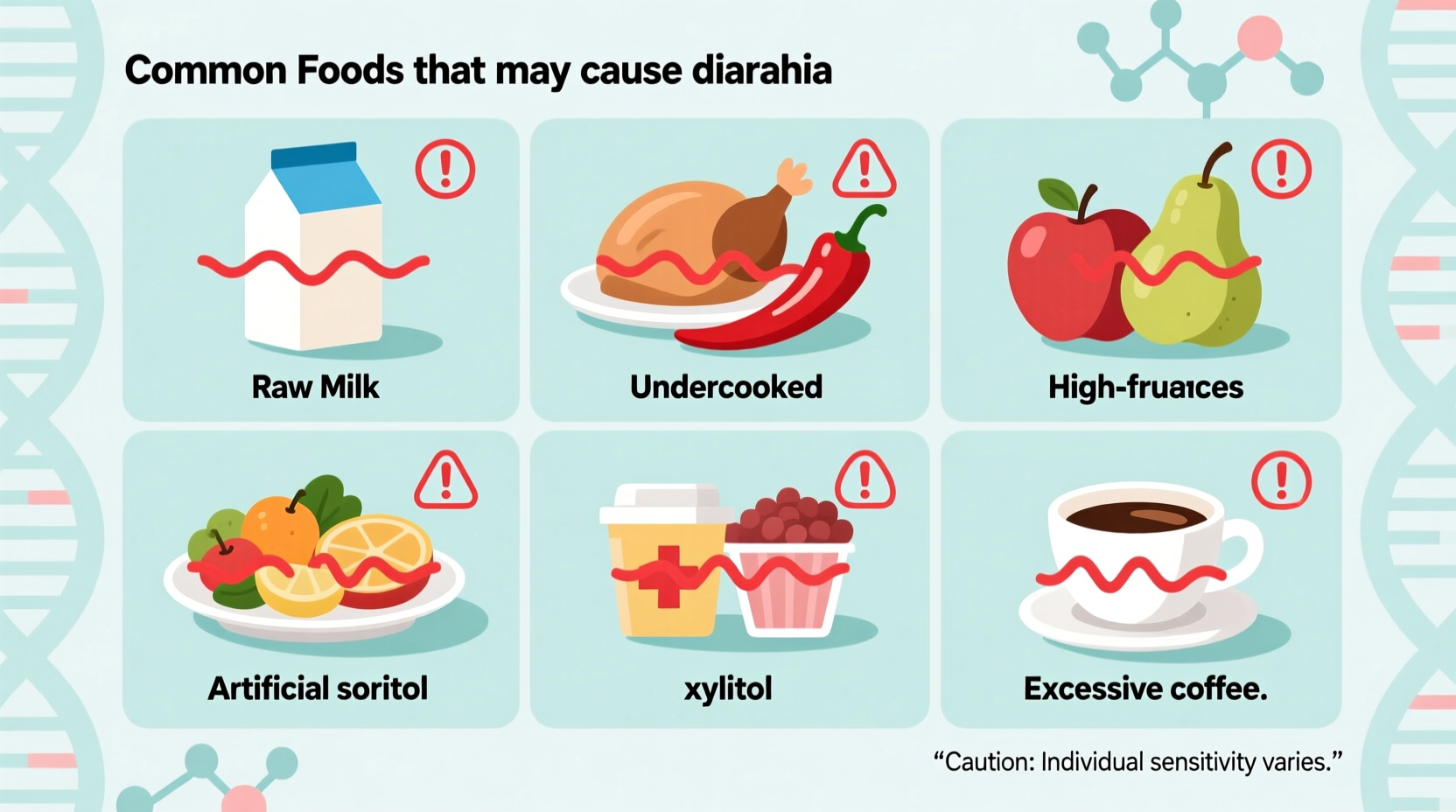
Approximately 68% of the global population experiences some degree of lactose intolerance, according to the National Institute of Diabetes and Digestive and Kidney Diseases. When lactase enzyme production decreases, undigested lactose ferments in the colon, causing bloating, cramps, and watery stools within 30 minutes to 2 hours after consumption. Common triggers include:
- Whole milk (contains highest lactose concentration)
- Ice cream and frozen desserts
- Soft cheeses like ricotta and cottage cheese
- Custards and puddings
Artificial Sweeteners and Sugar Alcohols
Sorbitol, mannitol, xylitol, and other sugar alcohols create an osmotic effect in the intestines, drawing water into the bowel and accelerating transit time. The U.S. Food and Drug Administration notes these compounds are common in "sugar-free" products but can cause significant digestive upset even in small quantities. Watch for these in:
- Sugar-free gums and mints
- Dietetic candies and chocolates
- "Light" or "reduced sugar" processed foods
- Some medications and supplements
High-Fat and Greasy Foods
Fried foods and high-fat meals can overwhelm the digestive system, particularly in individuals with compromised gallbladder function or pancreatic enzyme production. When fat isn't properly emulsified, it reaches the colon undigested, triggering the release of fluid and causing oily, foul-smelling diarrhea. Common offenders include:
- Fried chicken and other deep-fried items
- Heavy cream sauces and gravies
- Processed meats like sausages and bacon
- Fast food burgers and french fries
| Food Category | Common Triggers | Typical Reaction Time | At-Risk Populations |
|---|---|---|---|
| Dairy | Milk, ice cream, soft cheeses | 30-120 minutes | Lactose intolerant individuals |
| Sugar Alcohols | Sorbitol, xylitol, mannitol | 30-90 minutes | All consumers, especially sensitive individuals |
| High-FODMAP Foods | Apples, pears, onions, garlic | 2-6 hours | IBS sufferers, sensitive digestive systems |
| Spicy Foods | Chili peppers, hot sauces | 1-3 hours | Individuals with sensitive GI tracts |
Why Certain Foods Trigger Digestive Reactions
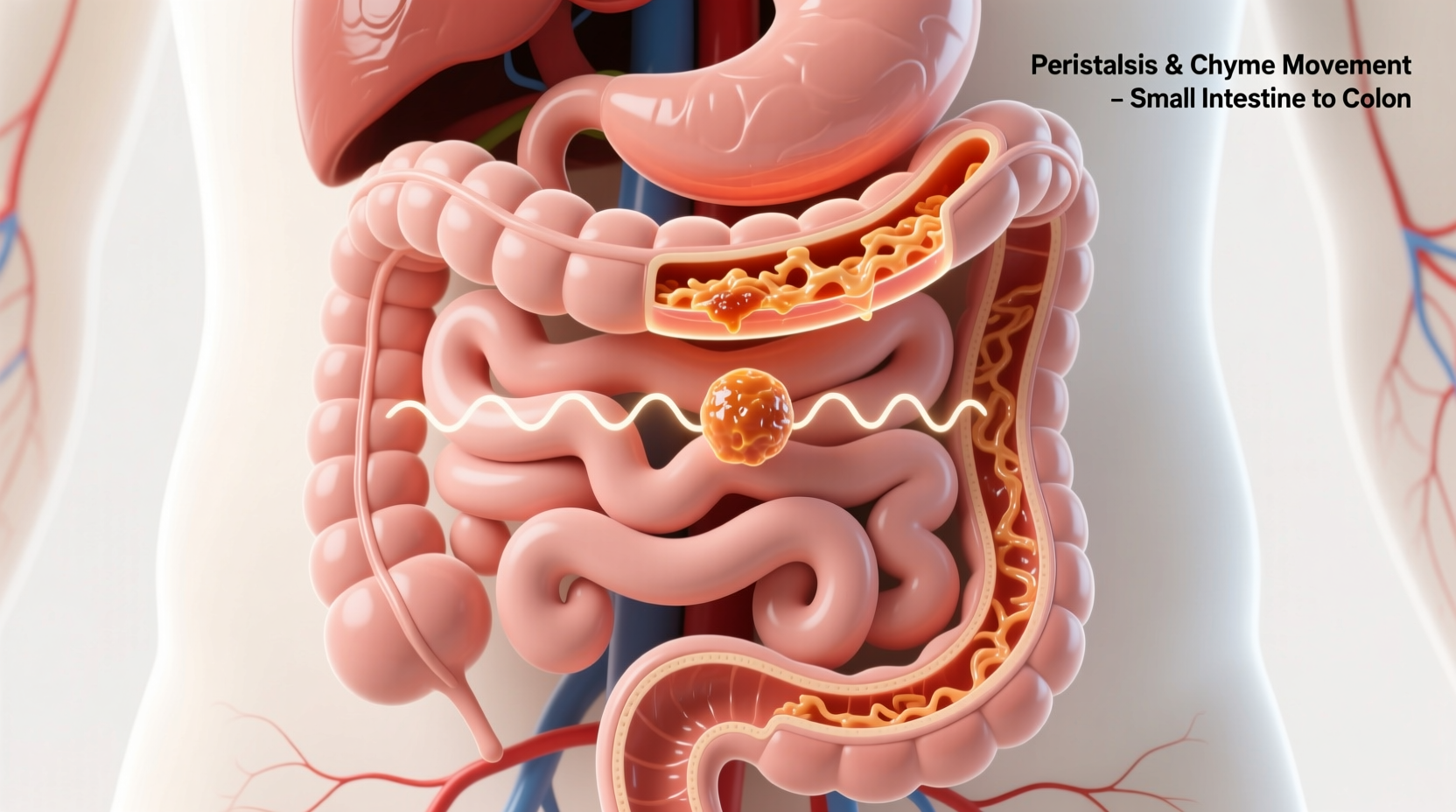
The digestive system responds to problematic foods through several physiological mechanisms. Lactose intolerance stems from enzyme deficiency, while sugar alcohols create osmotic pressure that pulls water into the bowel. Spicy foods containing capsaicin stimulate TRPV1 receptors throughout the digestive tract, accelerating motility. High-fat foods require adequate bile production for proper digestion—when this process falters, fat malabsorption occurs.
Research published in the American Journal of Gastroenterology shows that FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) can cause significant digestive distress in sensitive individuals. These short-chain carbohydrates ferment rapidly in the colon, producing gas and drawing water into the bowel.
Identifying Your Personal Food Triggers
Everyone's digestive system responds differently to potential triggers. The most effective approach to identifying your specific sensitivities involves:
Food Journaling Methodology
Maintain a detailed log for 2-4 weeks noting:
- All foods and beverages consumed (including brands and preparation methods)
- Timing of consumption relative to symptoms
- Specific symptoms experienced and their severity
- Stress levels and other potential contributing factors
Elimination Diet Protocol
Work with a healthcare provider to implement a structured elimination diet:
- Remove common trigger foods for 2-4 weeks
- Reintroduce one food category at a time (every 3-5 days)
- Monitor symptoms carefully during reintroduction phase
- Document reactions to identify specific triggers
When Food-Related Diarrhea Requires Medical Attention
While occasional digestive upset is common, certain symptoms warrant professional evaluation. Contact a healthcare provider if you experience:
- Diarrhea lasting more than 2 days without improvement
- Signs of dehydration (dark urine, dizziness, extreme thirst)
- Blood or black stools
- Severe abdominal or rectal pain
- Fever above 102°F (38.9°C)
- Unintended weight loss
The Centers for Disease Control and Prevention emphasizes that persistent diarrhea could indicate underlying conditions requiring medical intervention, including inflammatory bowel disease, celiac disease, or chronic infections.
Practical Strategies for Managing Food-Related Digestive Issues
Implement these evidence-based approaches to reduce digestive discomfort:
Dietary Modifications
- Choose lactose-free dairy alternatives or enzyme supplements
- Limit artificial sweeteners and sugar alcohols
- Opt for lean proteins and cooking methods like baking or steaming
- Gradually increase fiber intake to regulate bowel function
- Stay hydrated with electrolyte-balanced fluids
Lifestyle Adjustments
- Eat smaller, more frequent meals to reduce digestive load
- Chew food thoroughly to aid digestion
- Manage stress through mindfulness techniques
- Consider probiotic-rich foods to support gut microbiome
- Avoid eating large meals right before physical activity
Preventing Food-Related Digestive Emergencies
When traveling or dining out, implement these preventive measures:
- Research restaurant menus in advance for safe options
- Carry digestive enzyme supplements if needed
- Communicate dietary needs clearly to restaurant staff
- Have over-the-counter remedies available as backup
- Know restroom locations when away from home
Frequently Asked Questions
Can coffee cause diarrhea?
Yes, coffee can trigger diarrhea in sensitive individuals. Caffeine stimulates colonic activity, while coffee's natural acids can irritate the digestive tract. The National Institutes of Health reports that coffee increases gastrointestinal motility within 4-5 minutes of consumption, potentially causing urgent bowel movements in some people.
How long after eating does food-induced diarrhea typically occur?
Reaction times vary by trigger: lactose intolerance symptoms typically appear within 30-120 minutes; artificial sweeteners within 30-90 minutes; food poisoning pathogens may take 4-48 hours; and FODMAP reactions often manifest 2-6 hours after consumption. The Mayo Clinic notes that symptom timing helps identify the specific cause of digestive distress.
Are there foods that can help stop diarrhea?
Yes, the BRAT diet (bananas, rice, applesauce, toast) has been clinically shown to help firm stools. Additional beneficial foods include boiled potatoes, oatmeal, and clear broths. The UpToDate clinical resource recommends continuing normal feeding while avoiding dairy, fatty foods, and high-sugar items during recovery. Probiotic-rich foods like yogurt with live cultures can also help restore healthy gut bacteria.
Yes, sudden onset of diarrhea after eating specific foods could indicate food intolerance, allergy, or sensitivity. The American College of Allergy, Asthma, and Immunology distinguishes between food allergies (immune response with immediate symptoms) and intolerances (digestive system response with delayed symptoms). Consult a healthcare provider for proper testing and diagnosis if you experience consistent reactions to specific foods.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4