If you're monitoring uric acid levels due to gout or kidney concerns, knowing which foods to limit is essential. This guide delivers evidence-based information about purine-rich foods that elevate uric acid, plus practical dietary strategies backed by rheumatology experts. You'll learn exactly which foods impact uric acid production, how much matters, and smarter alternatives for balanced nutrition.
Understanding Uric Acid and Dietary Impact
Uric acid forms when your body breaks down purines—natural compounds found in certain foods and produced internally. While some uric acid is normal, excess levels (hyperuricemia) can crystallize in joints, causing painful gout attacks, or form kidney stones. The American College of Rheumatology confirms that dietary choices significantly influence uric acid production, though genetics and kidney function also play roles.
Crucially, most foods don't contain uric acid directly—they contain purines that convert to uric acid during digestion. This distinction matters because not all high-purine foods affect everyone equally. Let's examine the evidence on specific food categories.
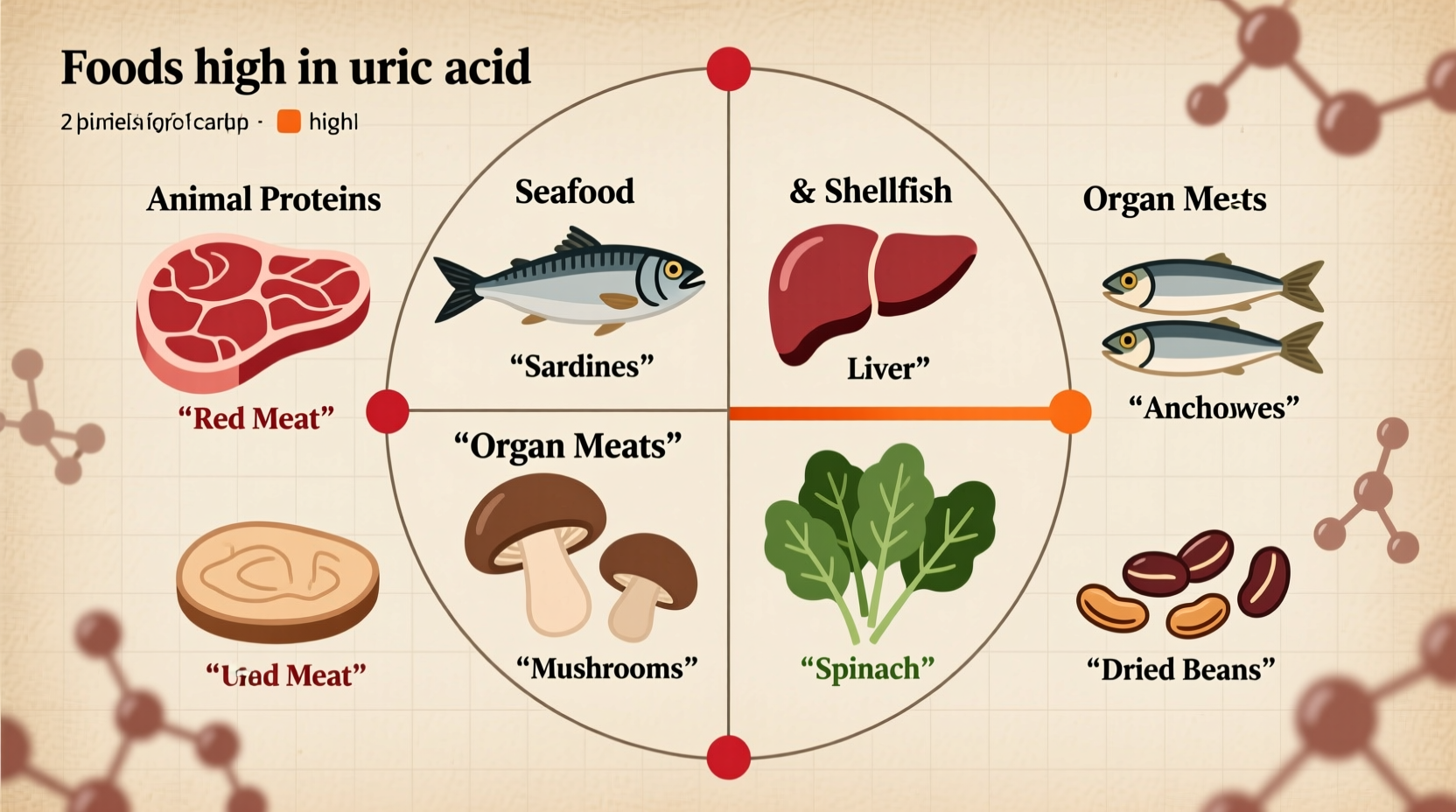
Foods Highest in Purines: What the Research Shows
Medical studies consistently identify these food groups as major purine sources. The Mayo Clinic categorizes purine-rich foods by concentration, helping you prioritize dietary changes.
| Food Category | Specific Examples | Purine Content (mg/100g) | Dietary Recommendation |
|---|---|---|---|
| Organ Meats | Liver, kidney, sweetbreads | 200-400 | Avoid completely |
| Seafood | Anchovies, sardines, mussels, scallops | 150-350 | Limited to 3-4 oz once weekly |
| Red Meats | Beef, lamb, venison | 100-200 | Limit to 4-6 oz, 2-3x weekly |
| Alcohol | Beer, hard liquor | N/A (inhibits excretion) | Avoid or strictly limit |
| Plant Foods | Asparagus, spinach, mushrooms | 50-150 | Generally safe in moderation |
Why Organ Meats and Certain Seafood Pose Highest Risk
Organ meats contain exceptionally high purine concentrations—up to 400mg per 100g serving. Research published in Arthritis & Rheumatology shows that frequent consumption increases gout flare risk by 50% compared to low-purine diets. Seafood like anchovies and sardines similarly overload the purine pathway, with one 3-ounce serving containing more purines than most daily recommendations.
The National Institutes of Health explains that animal-based purines convert to uric acid more efficiently than plant-based ones. This is why asparagus or spinach—while moderately high in purines—rarely trigger gout in most people, unlike organ meats.
Alcohol and Sugary Drinks: Hidden Uric Acid Triggers
Beer deserves special attention—it contains purines from yeast and inhibits uric acid excretion. A CDC analysis found beer consumption increases gout risk 2.5x more than spirits. Even moderate intake (2 servings daily) raises serum uric acid by 10-15%.
Sugary beverages pose another risk. High-fructose corn syrup in sodas and sweetened juices boosts uric acid production by increasing ATP breakdown. The American Journal of Clinical Nutrition reports that daily soda drinkers have 44% higher gout incidence than non-drinkers.
Practical Dietary Strategies Backed by Experts
Complete elimination of purine-rich foods isn't always necessary. The Arthritis Foundation recommends these evidence-based approaches:
- Portion control: Limit high-purine meats to 4 ounces (about deck-of-cards size) 1-2 times weekly
- Smart substitutions: Replace organ meats with lean poultry; choose low-purine fish like salmon instead of sardines
- Hydration focus: Drink 8-10 glasses of water daily to help kidneys flush uric acid
- Vitamin C boost: 500mg daily from foods like oranges may lower uric acid by 5% (per Mayo Clinic)
Remember that individual tolerance varies. The American College of Rheumatology advises tracking your food intake alongside symptoms for 4-6 weeks to identify personal triggers.
Evidence-Based Context: What Research Reveals
A 10-year study tracking 47,000 men (New England Journal of Medicine) found that those consuming two or more sugar-sweetened sodas daily had nearly double the gout risk compared to monthly drinkers. Meanwhile, moderate vegetable consumption—even purine-rich varieties—showed no significant association with increased flares.
This aligns with clinical guidance emphasizing that animal-based purines pose greater risk than plant-based sources. The key isn't eliminating all purines but managing high-risk categories while maintaining balanced nutrition.
Your Action Plan for Managing Uric Acid Through Diet
Start with these practical steps:
- Replace beer with wine (in moderation) or non-alcoholic alternatives
- Swap organ meats for lean protein sources like eggs or tofu
- Choose low-purine vegetables (carrots, cucumbers) over high-purine options when experiencing active flares
- Limit sugar-sweetened beverages to special occasions
- Consult a registered dietitian specializing in metabolic conditions for personalized plans
Diet alone won't cure gout, but research shows it can reduce flare frequency by 30-40% when combined with medical treatment. Always coordinate dietary changes with your healthcare provider, especially if taking uric acid-lowering medications.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4