Discovering you might have a food allergy can be overwhelming, but knowing exactly how to test for food allergies properly is your first step toward safe management. Unlike popular misconceptions, reliable food allergy diagnosis requires medical expertise and evidence-based testing protocols - not quick fixes or at-home kits. This guide walks you through the scientifically validated testing process, what to expect at each stage, and how to avoid potentially harmful misinformation.
Your Food Allergy Testing Journey: From Suspicion to Diagnosis
When food reactions concern you, understanding the proper diagnostic pathway prevents wasted time and potential health risks. The American College of Allergy, Asthma & Immunology (ACAAI) emphasizes that accurate food allergy testing begins with a detailed medical history before any physical tests occur. Your allergist will examine your symptoms, timing, and potential triggers to determine which evidence-based tests are appropriate for your specific situation.
Step 1: Recognizing Symptoms That Warrant Testing
Before pursuing food allergy testing methods, confirm your symptoms align with true IgE-mediated food allergies. These typically appear within minutes to two hours and may include:
- Hives or skin rash
- Swelling of lips, face, or throat
- Nausea, vomiting, or diarrhea
- Difficulty breathing or wheezing
- Anaphylaxis (severe, life-threatening reaction)
Non-IgE reactions (like food protein-induced enterocolitis syndrome) have different timelines and require specialized evaluation. The National Institute of Allergy and Infectious Diseases (NIAID) warns that self-diagnosis often confuses food allergies with intolerances or other conditions, leading to unnecessary dietary restrictions.
Step 2: Consulting the Right Specialist
Seek evaluation from a board-certified allergist - physicians with specialized training in diagnosing and managing allergies. The American Academy of Allergy, Asthma & Immunology (AAAAI) maintains a find-an-allergist directory to verify credentials. During your initial consultation, expect your specialist to:
- Review your complete symptom history
- Assess family allergy history
- Determine if testing is necessary based on symptom patterns
- Explain which specific tests might be appropriate for your case
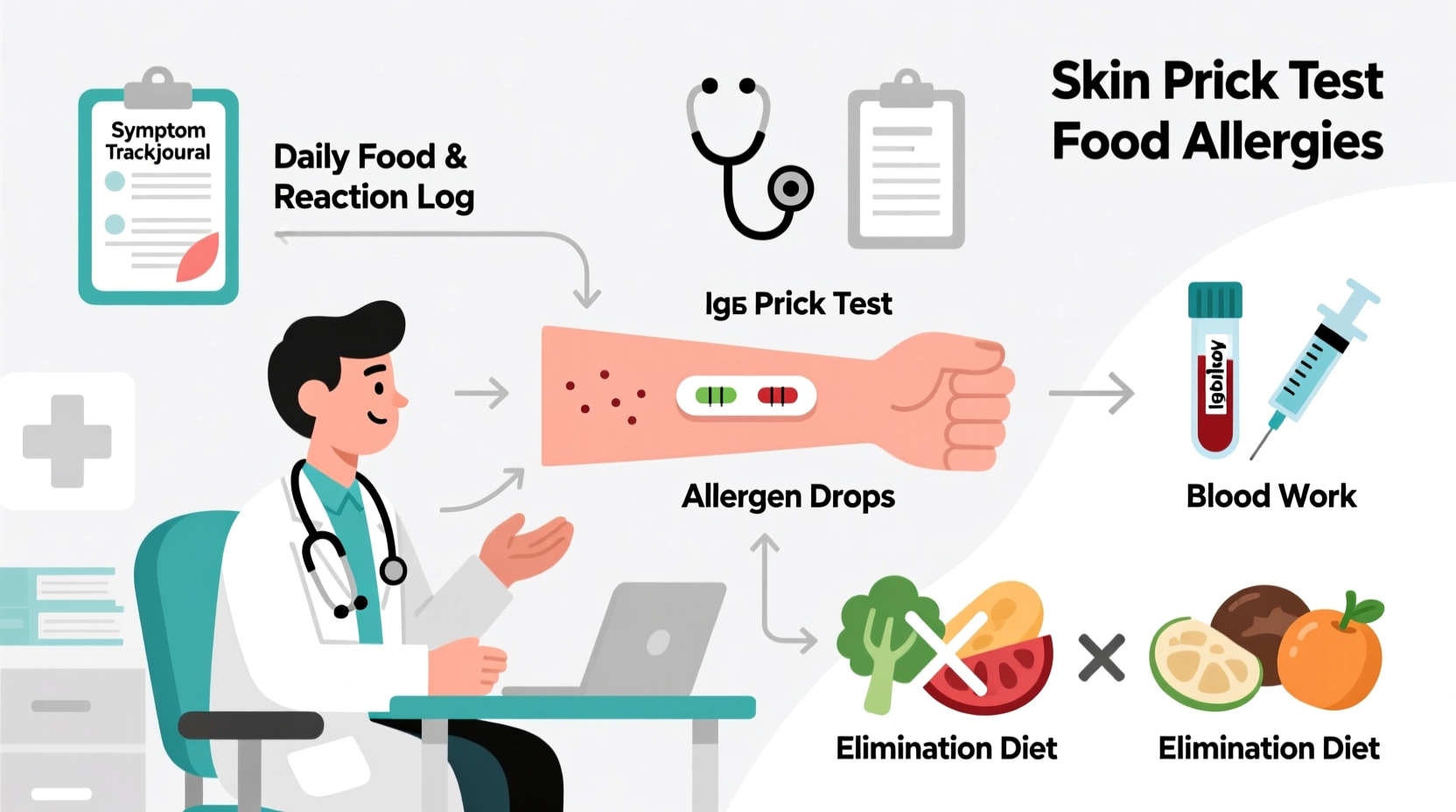
Step 3: Understanding Validated Testing Methods
Medically accepted food allergy diagnostic testing includes four evidence-based approaches:
| Test Type | How It Works | Accuracy Rate | Best For |
|---|---|---|---|
| Skin Prick Test | Small amounts of allergens placed on skin via pricks | 50-60% positive predictive value | Initial screening for common allergens |
| Specific IgE Blood Test | Measures allergen-specific antibodies in blood | Varies by allergen (peanut 95%, milk 76%) | Patients who can't stop antihistamines or have skin conditions |
| Oral Food Challenge | Gradual consumption of suspected food under medical supervision | Gold standard (near 100%) | Confirming diagnosis or checking for resolution |
| Supervised Elimination Diet | Removing then reintroducing suspect foods with medical guidance | High when properly conducted | Non-IgE mediated reactions or multiple food suspicions |
This comparison of reliable food allergy testing procedures comes from clinical practice parameters published by the NIAID. Note that no single test provides definitive answers - your allergist will interpret results in context with your medical history.
Step 4: What to Expect During Testing
Your food allergy testing experience follows a structured medical protocol:
- Pre-Testing Preparation: You'll receive instructions about medication adjustments (like stopping antihistamines before skin testing) and what to bring to your appointment
- Testing Session: Skin tests take 15-20 minutes with immediate results; blood tests require lab work with results in days
- Oral Challenge Protocol: Conducted over 3-6 hours with incremental food doses under constant medical supervision
- Results Interpretation: Your allergist explains findings in context of your history - positive tests alone don't confirm clinical allergy
- Management Plan: If diagnosed, you'll receive personalized guidance including emergency protocols
The Mayo Clinic emphasizes that proper diagnosis requires this comprehensive approach because up to 50-90% of presumed food allergies aren't confirmed by testing.

Avoiding Dangerous Testing Misinformation
Many commercial food sensitivity testing options lack scientific validation. The ACAAI explicitly warns against:
- IgG blood tests: Measure normal immune responses, not allergies (American College of Allergy, Asthma & Immunology position statement)
- Applied kinesiology: Muscle testing has zero diagnostic value for allergies
- Hair analysis: No scientific basis for detecting food allergies
- At-home test kits: Often inaccurate and lack professional interpretation
Research published in the Journal of Allergy and Clinical Immunology shows these unproven methods lead to unnecessary dietary restrictions in 82% of cases, potentially causing nutritional deficiencies. The CDC reports that misdiagnosis through unreliable testing increases anxiety and reduces quality of life without addressing actual health concerns.
Post-Testing: Building Your Management Strategy
After confirming food allergies through proper testing, work with your allergist to develop:
- Personalized avoidance strategies for your specific triggers
- Emergency action plan including epinephrine auto-injector training
- Nutritional guidance to maintain balanced diet while avoiding allergens
- Follow-up schedule to monitor potential allergy resolution (common in children)
Remember that food allergy management is dynamic - regular re-evaluation ensures your approach remains appropriate as your condition may change over time. The AAAAI recommends annual follow-ups for children and biennial check-ins for adults to assess potential allergy resolution.
Finding Trusted Resources for Ongoing Support
After completing food allergy diagnostic testing, rely on these authoritative sources:
- Food Allergy Research & Education (FARE): Evidence-based patient resources
- American Academy of Allergy, Asthma & Immunology: Find specialists and patient education
- National Institute of Allergy and Infectious Diseases: Clinical guidelines and research updates










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4