Food poisoning is a specific type of gastroenteritis caused by consuming contaminated food, while gastroenteritis (often called 'stomach flu') has broader causes including viruses, bacteria, and other pathogens. The critical differences lie in symptom onset (food poisoning typically appears within 1-6 hours versus 12-72 hours for viral gastro), specific causes, and sometimes symptom patterns. Knowing these distinctions helps determine appropriate treatment and when to seek medical care.
When sudden stomach cramps, vomiting, or diarrhea strike, understanding whether you're dealing with gastroenteritis or food poisoning can significantly impact your recovery. This guide provides medically accurate information to help you distinguish between these commonly confused conditions, recognize warning signs, and make informed decisions about your care.
Immediate Assessment: What to Do Right Now
If you're experiencing gastrointestinal symptoms, your first priority should be hydration and symptom monitoring. Both conditions cause fluid loss, but the urgency differs based on the cause. Start by noting:
- Exact time symptoms began appearing
- Specific foods consumed in the past 72 hours
- Temperature readings (fever suggests infection)
- Presence of blood in vomit or stool
According to the Centers for Disease Control and Prevention, documenting these details helps healthcare providers determine whether you're experiencing food poisoning (typically rapid onset after specific meal) or viral gastroenteritis (more gradual development).
Understanding the Medical Differences
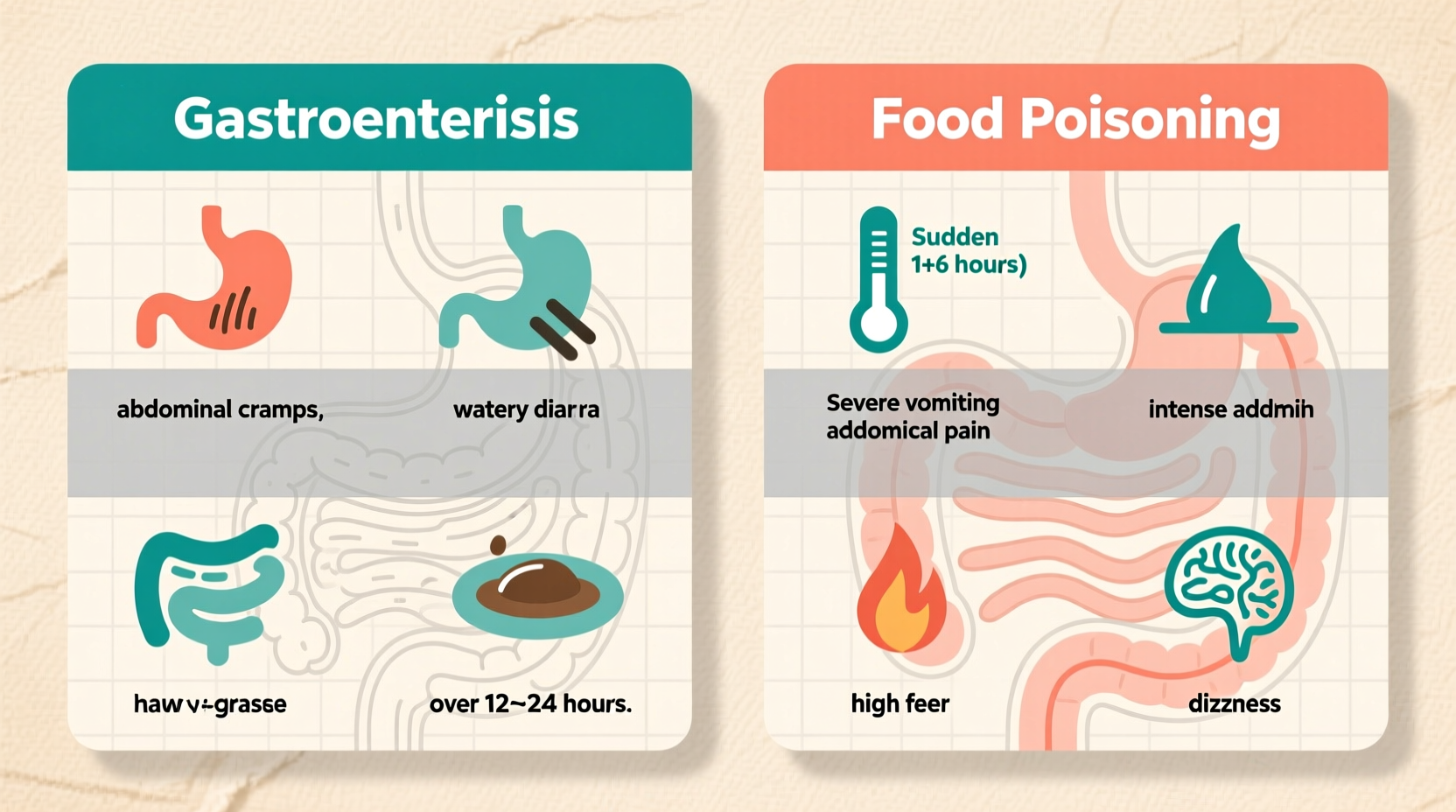
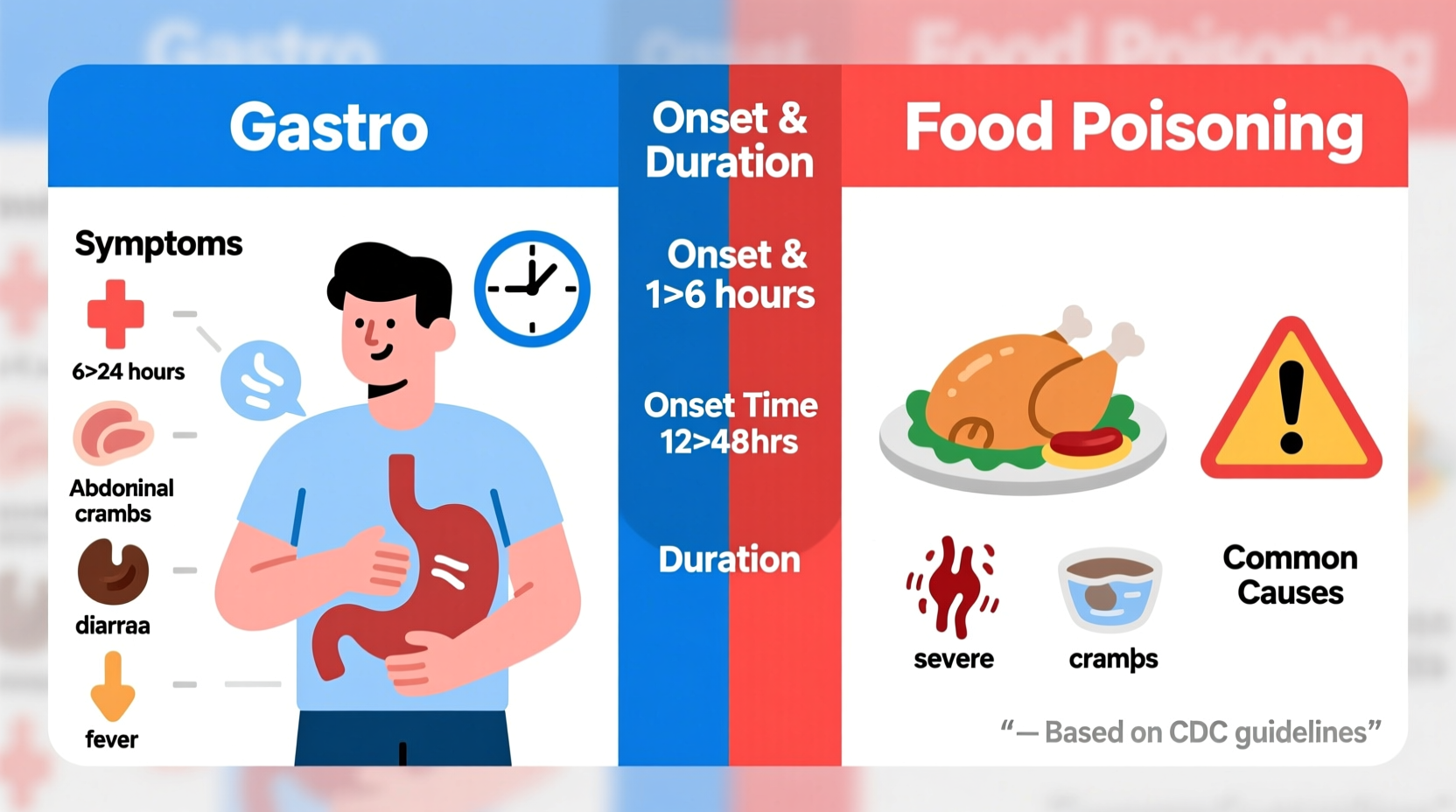
While both conditions affect the gastrointestinal system, their origins and characteristics differ significantly:
| Characteristic | Food Poisoning | Gastroenteritis |
|---|---|---|
| Primary Cause | Consuming contaminated food (bacteria, toxins, parasites) | Viral infection (norovirus, rotavirus), bacteria, or other pathogens |
| Symptom Onset | 1-6 hours after exposure | 12-72 hours after exposure |
| Duration | Usually 1-2 days | Viral: 1-3 days; Bacterial: up to 10 days |
| Common Symptoms | Sudden vomiting, cramps, diarrhea; often no fever | Gradual nausea, vomiting, diarrhea; frequently includes fever |
| Contagiousness | Not contagious (affects only those who ate contaminated food) | Highly contagious (spreads person-to-person) |
Symptom Timeline Analysis: When Symptoms Appear Matters Most
The timing of symptom appearance provides the most reliable differentiation between these conditions. As documented by the UK National Health Service, food poisoning symptoms typically manifest within hours of consuming contaminated food:
- 1-6 hours: Suggests toxin-mediated food poisoning (Staphylococcus, Bacillus cereus)
- 6-24 hours: Indicates bacterial infection (Salmonella, E. coli)
- 12-72 hours: More likely viral gastroenteritis (norovirus)
- 1-3 weeks: Could indicate parasitic infection (Giardia)
This timeline helps medical professionals determine appropriate testing and treatment. For example, rapid-onset symptoms often require different interventions than those appearing after a day or more.
Home Care Strategies: Tailored Approaches
While both conditions require hydration, your approach should differ based on the likely cause:
For Suspected Food Poisoning
- Stop eating temporarily (4-6 hours) to let your stomach settle
- Begin with small sips of electrolyte solutions, not plain water
- Keep packaging of suspected food for potential testing
- Avoid anti-diarrheal medications initially (they can trap toxins)
For Suspected Viral Gastroenteritis
- Focus on gradual rehydration with oral rehydration solutions
- Practice strict hand hygiene to prevent spreading to others
- Disinfect surfaces with bleach-based cleaners
- Consider probiotics to restore gut flora after symptoms subside
The Mayo Clinic emphasizes that attempting to stop diarrhea completely can prolong recovery, as your body is trying to eliminate pathogens.
Critical Warning Signs Requiring Immediate Medical Attention
While most cases resolve with home care, certain symptoms indicate serious complications. Seek emergency care if you experience:
- Signs of severe dehydration (dark urine, dizziness when standing, no urine for 8+ hours)
- Blood in vomit or stool (resembles coffee grounds or is bright red)
- High fever (over 101.5°F or 38.6°C) that doesn't respond to medication
- Symptoms lasting longer than 3 days without improvement
- Inability to keep fluids down for 12+ hours
These warning signs apply to both conditions but may indicate complications like kidney failure from E. coli infection or severe electrolyte imbalances requiring intravenous treatment.
Prevention Strategies: Reducing Your Risk
Understanding the differences informs better prevention:
Food Poisoning Prevention
- Follow proper food temperature guidelines (keep cold foods cold, hot foods hot)
- Wash hands thoroughly before handling food
- Cook meats to recommended internal temperatures
- Refrigerate leftovers within 2 hours
Gastroenteritis Prevention
- Get recommended vaccines (rotavirus vaccine for children)
- Practice thorough handwashing with soap for 20 seconds
- Avoid sharing utensils or drinks with sick individuals
- Disinfect high-touch surfaces during outbreaks
According to the World Health Organization, proper hand hygiene alone can reduce diarrheal disease risk by 30-48%, making it the single most effective prevention strategy.
When to Consult a Healthcare Professional
While many cases resolve with home care, consult a healthcare provider if:
- You cannot distinguish between the conditions and symptoms persist
- You belong to a high-risk group (infants, elderly, immunocompromised)
- You've recently traveled internationally
- You've consumed high-risk foods (raw shellfish, undercooked meats)
- You experience neurological symptoms (tingling, weakness)
Healthcare providers can perform tests to identify specific pathogens, which is crucial for proper treatment and preventing community spread.
Common Misconceptions Clarified
Several myths persist about these conditions that can lead to improper treatment:
- Myth: Antibiotics cure all stomach illnesses Fact: Antibiotics only work for bacterial infections and can worsen viral cases
- Myth: The '24-hour flu' is influenza Fact: True influenza affects respiratory system; 'stomach flu' is gastroenteritis
- Myth: Food poisoning always comes from restaurants Fact: Most cases originate from home food handling errors
- Myth: Clearing your stomach with ipecac helps Fact: Medical professionals no longer recommend ipecac for food poisoning
Practical Summary: Your Action Plan
When gastrointestinal symptoms strike, follow this practical approach:
- Document: Note exact symptom onset time and recent food consumption
- Hydrate: Begin small sips of electrolyte solution immediately
- Assess: Check for warning signs requiring emergency care
- Differentiate: Use onset timing to determine likely cause
- Act: Implement appropriate home care strategy
- Monitor: Track symptoms for improvement or warning signs
This systematic approach ensures you're addressing your specific condition effectively while recognizing when professional medical care becomes necessary.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4