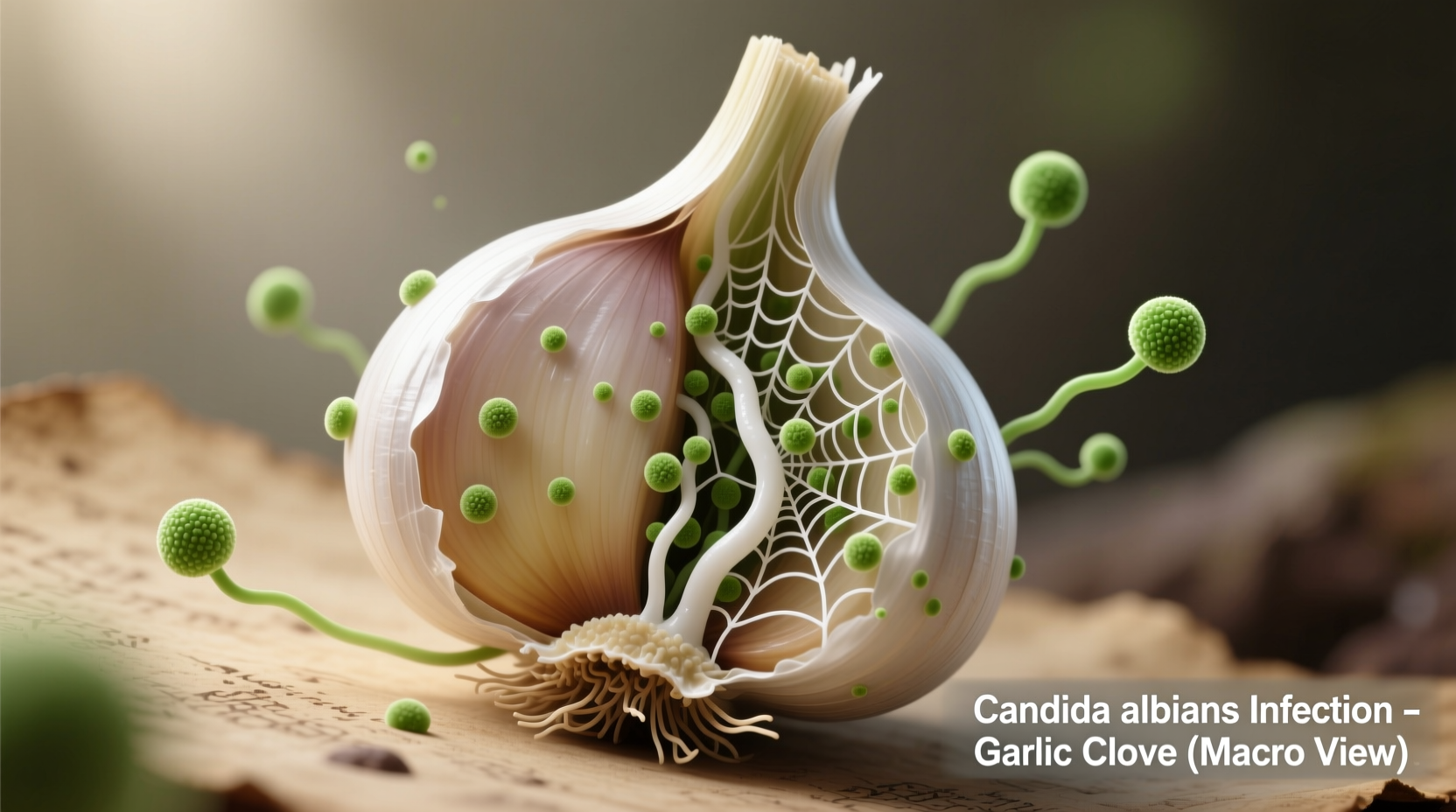
When exploring natural approaches to Candida management, many people wonder about garlic's potential benefits. This comprehensive analysis examines what current research reveals about garlic's antifungal properties and their practical application for Candida concerns. We'll separate evidence-based findings from common misconceptions while providing actionable guidance for those considering garlic as part of their wellness strategy.
The Science Behind Garlic and Candida
Garlic (Allium sativum) contains allicin, the primary bioactive compound formed when garlic is crushed or chopped. According to research published in Frontiers in Microbiology, allicin demonstrates significant antifungal activity against Candida albicans by disrupting fungal cell membranes and inhibiting essential enzymes. A 2020 laboratory study at the University of Maryland found that allicin reduced Candida growth by 72% at concentrations achievable through dietary consumption.
However, it's crucial to understand that laboratory results don't always translate directly to human effectiveness. The National Center for Complementary and Integrative Health (NCCIH) notes that while garlic shows promise as a complementary approach, "current evidence is insufficient to recommend garlic as a primary treatment for fungal infections."
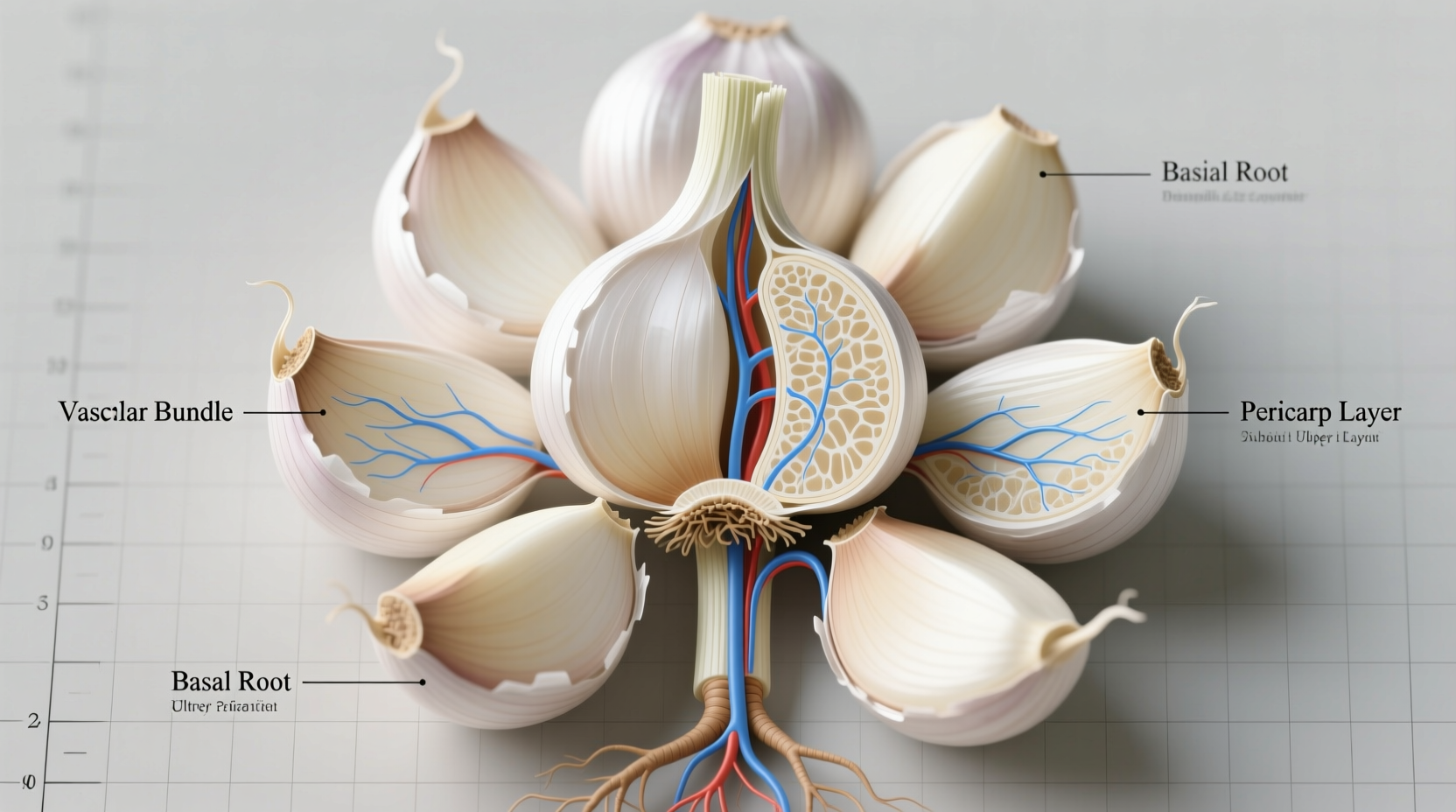
How Garlic Works Against Candida
Garlic's antifungal mechanism involves multiple pathways:
- Cell membrane disruption - Allicin damages Candida cell walls, causing leakage of cellular contents
- Enzyme inhibition - Interferes with sulfur-containing enzymes essential for fungal metabolism
- Biofilm prevention - Reduces Candida's ability to form protective colonies on surfaces
- Immune modulation - Enhances white blood cell activity against fungal invaders
Practical Application Guidelines
For those considering garlic as complementary support, proper usage matters significantly:
| Method | Preparation | Frequency | Notes |
|---|---|---|---|
| Raw consumption | 1-2 cloves crushed, allowed to sit 10 minutes before eating | Once daily with food | Maximizes allicin formation; may cause digestive discomfort |
| Aged garlic extract | Standardized supplements (1.2-2.4 mg SAC) | As directed on label | Milder on stomach; consistent dosing |
| Garlic oil | Diluted (1:10 with carrier oil) | Topical application 2x daily | For skin yeast infections only; patch test first |
Important Limitations and Considerations
Understanding the boundaries of garlic's effectiveness prevents unrealistic expectations:
- Not a replacement for medical treatment - Systemic Candida infections require prescription antifungals
- Dosage challenges - Therapeutic levels difficult to maintain consistently through diet alone
- Drug interactions - May enhance blood-thinning medications' effects (consult physician)
- Gastrointestinal sensitivity - Raw garlic can irritate digestive tract in some individuals
The Centers for Disease Control and Prevention (CDC) emphasizes that "while some natural products show antifungal properties in laboratory settings, clinical evidence supporting their effectiveness for treating human fungal infections remains limited." Serious Candida infections, particularly systemic cases, require professional medical treatment.
Garlic in Context: Complementary Approach
When considering garlic for Candida management, position it within a comprehensive strategy:
- Use alongside conventional treatment for mild cases under medical supervision
- Combine with dietary approaches that reduce sugar intake (Candida's primary food source)
- Pair with probiotic-rich foods to support healthy gut flora balance
- Consider as part of a short-term intervention rather than permanent solution
A 2022 review in the Journal of Fungi concluded that "garlic extracts demonstrate promising synergistic effects when combined with conventional antifungal medications, potentially reducing required pharmaceutical dosages and associated side effects." This suggests garlic's most valuable role may be as complementary support rather than standalone treatment.
When to Seek Professional Medical Care
Recognize symptoms requiring immediate medical attention:
- Persistent oral thrush lasting more than 2 weeks
- Recurrent vaginal yeast infections (4+ episodes yearly)
- Symptoms spreading beyond localized areas
- Signs of systemic infection (fever, chills, widespread rash)
The American Academy of Family Physicians states that "self-treatment of suspected fungal infections without proper diagnosis can lead to complications and delayed appropriate care, particularly when symptoms mimic other conditions." Always consult a healthcare provider for proper diagnosis before implementing any treatment strategy.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4